Contents
1 Policy summary
This policy informs colleagues, patients and visitors of the smoke free policy for Rotherham Doncaster and South Humber Trust (RDaSH). This policy was created to protect colleagues, visitors and patients from the harmful effects of smoking, whether that be first or second hand smoke. This policy outlines the support available to patients, colleagues and visitors.
2 Introduction
Smoking is a leading cause of preventable death in England. It is linked to diseases such as cancer, heart disease, and respiratory conditions. It also impacts mental health and can increase medication needs for those with mental health problems. In response, the government aims to reduce smoking prevalence to 5% by 2030, and the NHS plans to provide tobacco treatment services to all hospital admissions by 2024.
Hospitals should be smoke-free both indoors and outdoors to protect everyone from the harmful effects of smoking. This includes offering treatment to smokers who wish to quit and supporting those who do not wish to quit in managing their smoking while on trust premises.
2.1 Legal position
The trust is required by law to provide a safe environment free from health risks such as second-hand smoke. The Health and Safety at Work Act (1974) and the Health Act (2006) mandate smoke-free regulations, which apply to all trust premises, including buildings, grounds, and vehicles.
3 Purpose
This policy aims to:
- promote a smoke-free environment for all trust premises
- protect all individuals from the health risks of second-hand smoke
- safeguard colleagues from smoke exposure at work
- support patients and colleagues in quitting smoking by offering nicotine replacement and behavioural support
- allow colleagues to conduct searches to maintain a smoke-free environment, including random or routine searches of patients with unescorted leave (refer to the searching of a person (patient and visitor) or their property policy)
- reduce fire risks associated with smoking
4 Scope
This policy applies to all colleagues, patients, visitors, and others on trust premises or during RDaSH service delivery.
4.1 Exclusions
St John’s Hospice is exempt from the general smoke-free policy for patients, who may smoke in designated outdoor areas. Smoking is prohibited indoors. Patients at St John’s Hospice can access smoking cessation services. All other colleagues and visitors must comply with the smoke-free policy on hospice premises. All palliative community patients are requested to refrain from smoking indoors during home visits and for an hour before colleagues arrive.
5 Procedure
5.1 Quick guide
5.1.1 Key point 1
- RDaSH is a smoke free trust. Smoking is prohibited on all RDaSH sites (with an exemption for St John’s Hospice). This includes all indoor and outdoor areas. If colleague choose to smoke, they must do so off site and must not be identifiable as a health care worker. This means changing out of uniform and removing badges and lanyards.
5.1.2 Key point 2
- Vaping is permitted in outdoor areas for patients and visitors. Colleagues cannot vape on trust premises or in trust vehicles. Vaping is not permitted inside any trust buildings or buildings used for RDaSH appointments in the community.
5.1.3 Key point 3
- Patients are prohibited from smoking on escorted section 17 leave.
5.1.4 Key point 4
- Colleagues working in the community should request a smoke free environment when visiting a patient’s home. Arrangements should be made with patients prior to your visit to prevent the risk of second-hand smoke. Colleagues should request that patients and, or anyone else present refrain from smoking indoors during the visit and for an hour before colleagues arrive.
5.1.5 Key point 5
- All breaches of the smoke free policy should be reported via the Ulysses IR1 system.
5.1.6 General approach
- Promote and maintain a smoke-free environment.
- Offer tobacco treatment service support to patients and colleagues.
- An approach to discuss the smoke free policy should only be made once to avoid conflict. The trust will apply a no excuse for abuse approach to any individual who becomes abusive when reminded of the smoke free policy.
- Colleagues are expected to adhere to the principles taught in the trust’s conflict resolution and reducing restrictive interventions training courses.
5.2 Prohibited and permitted items
- Patients and visitors to trust premises will be made aware of the smoke free policy through signs, posters, leaflets and conversations with colleagues.
- Patients and visitors will be informed about prohibited items (tobacco, cigarettes, lighters) through signage and communication.
- Prohibited item issues should be addressed with visitors; visitors who provide prohibited items to patients will be asked to support the patient’s treatment plan in the first instance. Persistent offenders may be banned from future visits.
- Smoking paraphernalia should be stored securely in lockers; colleagues must not bring such items onto wards.
- For guidance on specific products, contact the QUIT team at quit@nhs.net.
6 Community services
6.1 Assessment
- During the initial assessment, document patients’ smoking habits using the trust smoking template on SystmOne (see appendix C)
- Questions should cover:
- current use of tobacco or e-cigarettes
- past attempts to quit and methods used
- reasons for past or current smoking habits
- refer all smoking patients to in-house smoking cessation support unless they opt out
- important, screen all community patients 18 years or older on registration or at least annually, including non-smokers
6.2 Referrals and treatment
- Review smoking status at least annually, or during dialog reviews.
- Where possible, carry health promotional materials about smoking cessation services.
- Where a patient is likely to have contact with inpatient services, inform patients about smoke-free inpatient services and that support to abstain from smoking will be offered during any inpatient stay.
- For referral pathways please see appendix D.
6.3 Visiting patients who smoke at home
- Request a smoke-free environment during home visits. include this request in appointment letters and verbal communications.
- Consider alternative arrangements if compliance is an issue:
- smoke in a separate room before visits
- use nicotine patches before or during appointments
- attend appointments at a clinic instead of home visits
- Include details of any alternative arrangements in the patient’s care plan.
- Review cases of persistent non-compliance and adjust the treatment plan as needed.
7 Inpatient services
7.1 Admission and assessment
- All trust inpatient wards and premises are smoke-free which includes all mental health wards. St John’s hospice is the only exception to this and provisions for this are stated in section 3.1 of this policy.
- Patients may vape outside while on site. this includes ward gardens or courtyards.
- Vaping in any indoor area is prohibited for all patients, colleagues and visitors.
- The above restrictions must be explained to patients and visitors before admission or soon as the patient arrives.
- Screen all patients within 24 hours of admission or readmission using the trust inpatient smoking screening questionnaire on SystmOne (see appendix E).
During admission:
- assess smoking status and past attempts to quit
- offer abstinence support and refer to the QUIT service
- for North Lincolnshire, refer to community services on discharge
- important, all inpatients, including non-smokers and those transferred from North Lincolnshire to a Doncaster or Rotherham care group, must be screened
- secure any smoking paraphernalia found on patients and store it in ward lockers, patients may access these items during unescorted leave but must surrender them upon return
- if patients refuse to hand over items, refer to the searching of a person or their property policy
- offer approved brief advice along with disposable vapes or nicotine replacement therapy, vapes cannot be given to anyone under the age of 18
- follow the QUIT approach:
- Q, ask and record smoking status
- U, understand addiction level
- I, inform about health benefits
- T, initiate treatment and refer to services
- if a patient declines cessation support, they must remain smoke-free on trust premises, a care plan should be developed for smokers detailing abstinence support during their stay
7.1.1 Trust supplied nicotine replacement therapy (NRT) and vapes
- All NRT is available to patients who smoke at any time during their admission, free of charge.
- Vapes are available to all patients who smoke, free of charge, for the first 72 hours of their admission after 72 hours, patients who are engaging with a quit attempt or reduction with the view to quit will be eligible for trust supplied vapes for a 12-week period.
- If a patient does not want to make a quit attempt, they will be offered other forms of NRT (lozenges, patches, inhalators) to support abstinence during their admission.
- Vapes must be transcribed or prescribed by colleagues and noted on the patients’ drug card.
- If at any point you are unsure about the appropriate NRT or vape for a patient, please contact a ward tobacco treatment advisor or the quit team.
7.2 Risk management on inpatient wards
- Assessment: all smokers should have a smoking risk assessment (see appendix F) and a risk management care plan.
- Key risks:
- covert smoking, especially in bed
- prohibited items (for example, ignition sources, cigarettes) brought onto the ward by visitors or by the patient after a period of leave
- increased risk of absconding
- risk of ingestion of vape batteries as self-harm
- Reference: see appendix G for management of chargeable vaping devices.
7.3 Medication management
- Impact of smoking: smoking affects drug metabolism, requiring dose adjustments when smoking status changes for some medications.
- Monitoring: closely monitor medication levels, especially for drugs with a narrow therapeutic index like clozapine. it is recommended that plasma levels of clozapine should be measured before smoking cessation commences, reducing the dose as needed and repeating plasma levels one week after cessation, to enable more accurate and timely monitoring and adjustment of medications.
- Resources: consult the specialist pharmacy service (opens in new window) or the trust pharmacy team for advice.
7.4 Section 136 assessments
- Vaping or NRT provision, offer approved disposable vapes or 24-hour NRT based on smoking habits:
- 21mg per 24 hours for greater than 10 cigarettes per day
- 14mg per 24 hours for less than 10 cigarettes per day
- Documentation: the use of this is to be recorded on the form prn nicotine replacement therapy NRT record of use.
7.5 Seclusion
- Nicotine replacement: offer NRT during seclusion; disposable and rechargeable vapes are not permitted in seclusion.
- Risk assessment: provide NRT based on individual risk assessments.
7.6 Visitors
- Policy: all visitors must adhere to the trust’s smoke free policy.
- Information: provide information about smoke free status of the trust in carer’s information packs or on arrival. if this is not possible, visitors should be informed of this on arrival.
- Storage: visitors must store smoking paraphernalia in lockers.
- Vaping: allowed only in outdoor areas.
7.7 Environmental management
- Routine checks: designate a colleague each shift to monitor compliance and check the environment.
- Removal: patients and visitors breaching the smoke free policy are responsible for clearing up any smoking related rubbish such as cigarette butts, packaging or ash that they have created. any that is not removed by those using it will be removed by facilities and domestic teams.
7.8 Access to information
- Display: wards must display health promotion materials on the harms of smoking and cessation support.
7.9 Non-compliance
- Action: for persistent non-compliance, conduct a multi-disciplinary team (MDT) review to determine actions and update the care plan. The trusts supportive observation of inpatients who are identified as posing a significant risk to themselves or others policy should be used for patients who are identified as posing a fire risk due to covert smoking.
- Support: discuss in ERICA and report non-compliance via the Ulysses IR1 system (see section 8.1).
7.10 Violence and aggression
- Handling: if a patient becomes violent or aggressive in relation to the smoke free policy, de-escalation is the preferred option. there is no expectation that colleagues should put themselves at risk.
- Protocol: follow the reducing restrictive interventions policy and ensure the patient make arrangements to avoid future breaches, which should be recorded in a car plan.
7.11 Section 17 leave
- Purpose: section 17 leave should not be used to facilitate smoking.
- Rationale: smoking or “smoking leave” has been found to add no therapeutic value to a patients care. smoking is known to increase symptoms of poor mental and physical health.
7.12 Discharge
- Discharge plan: patients should be asked if they wish to continue with support to stop smoking when they are discharged. if they would like support, it should be included in their discharge plan and the following steps should be followed:
- NRT and vapes: provide 2 weeks’ worth of NRT products or 1 weeks’ worth of vapes. post-discharge, the quit team will provide vapes
- referral: patients will be given a follow-up call once they leave hospital via from the quit team to offer to continue support post discharge
- notes: where a patient has stopped smoking, ensure that discharge notes make clear that blood plasma levels may be affected and may need to be adjusted
8 Breaches and reporting
8.1 Reporting smoking-related incidents
- Reporting: all breaches must be logged on the trust Ulysses ir1 system as per the trust incident management policy. This helps monitor trends and manage risks.
- Reporting categories:
- type of incident: security, loss, or damage
- cause group: security, loss, theft, or damage
- cause: smoking policy breach or concern
- Violence and aggression: if violence or aggression is involved, log the incident under violence and aggression with smoking as a secondary cause
- Responsibility: ward colleagues must report incidents or ask a manager to do so if they lack access to Ulysses
- Issues:
- report any issues with completing IR1s due to capacity to the ward manager and service manager or modern matron
- persistent non-compliance with the smoke free policy should be reported to the modern matron and service manager
- complaints should first be handled by the ward and team manager; unresolved issues can be escalated to pals or through the formal complaint’s procedure
8.2 Sale of tobacco products
- Prohibition: no tobacco sales are allowed on trust premises. selling, transporting, or possessing illegal tobacco products is a criminal offence.
- Enforcement: colleagues suspecting illegal tobacco on premises should search for and remove it. the trust will cooperate with law enforcement, and illegal activity by colleagues will result in disciplinary action.
9 Colleague support
9.1 Smoking cessation support
- Support: the trust offers up to 12 weeks of smoking cessation support per year for employees in Rotherham or Doncaster. Colleagues are able to access free NRT and vapes. North Lincolnshire colleagues should contact the North Lincolnshire Healthy Lifestyles Service.
- incentives: Colleagues who successfully quit can receive gift vouchers (£10 at 4 weeks, £30 at 12 weeks). To sign up, email either:
- Email: quit@nhs.net
- Email: healthandwellbeing@nhs.net
9.2 Workplace responsibilities
- Restrictions:
- colleagues must not smoke, chewing tobacco, or vape on trust grounds, inside trust premises, or inside trust vehicles. Colleagues who struggle with this can be referred to the colleague service at any time for support
- colleagues are not entitled to smoking or vaping breaks. If colleagues wish to vape or smoke this must be done during their allotted breaks and in accordance with the smoke free policy
- Uniform: no smoking or vaping in uniform or while identifiable as a health worker, irrespective of whether they are on duty or on trust premises. badges should be removed and clothes should be changed.
- Vehicles: smoking and vaping are prohibited in trust vehicles and while traveling with trust colleagues.
- Disciplinary: continued non-compliance may lead to disciplinary action.
9.3 Colleague breaches
- Expectations:
- colleagues should promote a smoke free environment and avoid condoning, facilitating or advocating tobacco smoking
- all trust colleagues are prohibited from purchasing or providing tobacco products for patients. colleagues must not use tobacco as a reward for patients
- breaches should be reported to line managers. repeated breaches may result in action through the trust disciplinary policy and personal responsibility framework
10 Training implications
10.1 Very brief advice training, all colleagues
- How often should this be undertaken: Every 3 years.
- Length of training: 30 minutes.
- Delivery method: Face-to-face or Microsoft Teams.
- Training delivered by whom: QUIT team.
- Where are the records of attendance held: Electronic staff record (ESR).
10.2 Transcribing nicotine replacement therapy (NRT), all colleagues issuing pharmacotherapy
- How often should this be undertaken: Every 3 years.
- Length of training: 30 minutes.
- Delivery method: Face-to-face or Microsoft Teams.
- Training delivered by whom: QUIT team.
- Where are the records of attendance held: Electronic staff record (ESR).
As a trust policy, all colleagues need to be aware of the key points that the policy covers. Colleagues can be made aware through:
A variety of means such as:
- all user emails for urgent messages
- one to one meetings or supervision
- continuous professional development sessions
- posters
- group supervision
- special meetings
- intranet
- team meetings
- local induction
- chief executive’s video log
- trust induction
11 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
11.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, “not just clinically but in terms of dignity and respect”.
Consequently, the trust is required to articulate its intent to deliver care with privacy and dignity that treats all patients with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity, and respect, (when appropriate this should also include how same sex accommodation is provided).
11.1.1 How this will be met
There are no additional requirements in relation to privacy, dignity and respect.
11.2 Mental Capacity Act (2005)
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals’ capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all employees working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason, all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected, and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
11.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act (2005) (section 1).
12 Links to any associated documents
- Physical health policy
- Supportive therapeutic observation policy
- Reducing restrictive interventions (RRI) policy (formerly prevention and management of violence and aggression (PMVA) policy)
- Searching of a person or their property policy
- Personal responsibility framework procedure
- Disciplinary policy
- Incident management policy
- Guidelines for nicotine management therapy and attached units (staff access only) (opens in new window)
13 References
- Department of Health and Social Care (2011) No Health Without Mental Health: a cross-government outcomes strategy (opens in new window).
- Department of Health and Social Care (2017) Smoke-free generation: tobacco control plan for England (opens in new window).
- Department of Health and Social Care (2017) Tobacco control plan: delivery plan 2017 to 2022 (opens in new window).
- Harker and Cheeseman (2016) The Stolen Years: Mental Health and Smoking Action Report, Action on Smoking and Health (ASH) (opens in new window).
- Health and Safety Executive (2020) Health and Safety at Work Act (1974) (opens in new window).
- Health and Safety Executive (2020) Health Act (2006) (opens in new window).
- NHS Digital (2018) Statistics on Smoking, England, 2018 (opens in new window).
- NICE (2021) Tobacco: preventing uptake, promoting quitting and treating dependence (opens in new window).
- NICE (2013) smoking: acute, maternity and mental health services, public health guideline (ph48) (opens in new window).
- NICE (2013) smoking: harm reduction (opens in new window).
- PHE (2020) health matters: smoking and mental health Public Health England guidance (opens in new window).
14 Appendices
14.1 Appendix A Responsibilities, accountabilities and duties
14.1.1 The trust
The trust has a duty of care and a duty of confidentiality to ensure that all aspects of healthcare record keeping are properly managed. The trust must adhere to the legislative, statutory, and good practice guidance requirements relating to healthcare records management.
14.1.2 The chief executive
- Is responsible for overall health, safety, and welfare of the trust.
- Has delegated this function is delegated to the chief operating officer and senior responsible officer who are accountable for policy implementation.
- Is responsible for ensuring the trust has effective policies and procedures for a smoke-free environment.
- Is responsible for oversee compliance with relevant legislation.
14.1.3 Executive director of nursing and allied health professionals, deputy director of nursing
- The deputy director of nursing, delegated by the executive director of nursing and AHP’s, oversees the QUIT program and ensures adherence to the policy.
14.1.4 Senior managers of the trust
The Health Act (2006) section 8 and sub section 1 states that ‘it is the duty of any person who controls or is concerned in the management of smoke free premises to cause a person smoking there to stop smoking’ and therefore directors, care group directors and managers are responsible for:
- raising awareness and ensuring effective communication of the policy
- ensuring screening of every patient within 24 hours of admission or registration and recording the status on SystmOne
- maintaining a safe, healthy environment by applying the policy
- addressing concerns and take action regarding non-compliance
- completing risk assessments for passive smoking exposure
- ensure patients are informed and supported in managing or quitting smoking
14.1.5 All employees
- Comply with and support the smoke-free policy.
- Report non-compliance incidents to line managers and via the trust ir1 incident reporting system.
- Notify managers of passive smoking incidents and request patients to smoke outside or to refrain from smoking inside for an hour before visits.
- Request that patients extinguish cigarettes and move away from trust premises.
- Prevent and manage ignition sources and smoking paraphernalia on trust premises.
- Be aware that persistent non-compliance may lead to disciplinary action in accordance with the trusts’ disciplinary policy.
14.2 Appendix B Monitoring arrangements
14.2.1 Policy implementation
- Who by: All managers.
- Reported to: Care group quality meetings.
- Frequency: As incidents arise.
14.2.2 Smoking related fire incidents
- Who by: Health and Safety team.
- Reported to: Health, safety and security forum.
- Frequency: Bi-monthly.
14.2.3 Non-fire smoking related incidents
- Who by: All managers.
- Reported to: Care Group Quality meetings.
- Frequency: Bi-monthly.
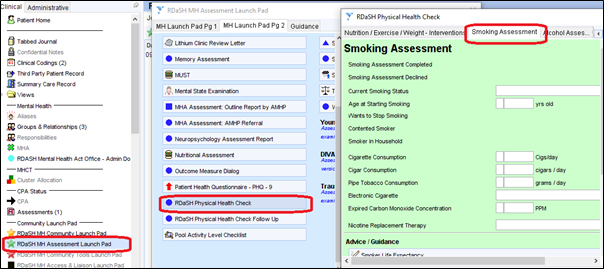
14.3 Appendix C Location of the trust smoking template for screening of mental health community services patients
Located under “RDaSH MH Assessment Launch Pad”, “RDaSH Physical Health Check”, then “Smoking Assessment”.
14.4 Appendix D Referral routes for trust community patients who opt into receiving smoking cessation support
14.4.1 Doncaster
14.4.1.1 Option 1 (preferred)
In-house quit service by either:
- using a referral form on SystmOne (see appendix H)
- Email: quit@nhs.net
14.4.1.2 Option 2
If option 1 is not available or patient explicitly states, they would like to be supported by an external service.
External Yorkshire smoke free service by contacting:
- Phone: 0800 612 0011
- Phone: 0330 660 1166
- Email: swy-tr.y-smokefree@nhs.net
14.4.2 Rotherham
14.4.2.1 Option 1 (preferred)
In-house quit service by either:
- using a referral form on SystmOne (see appendix H)
- Email: quit@nhs.net
14.4.2.2 Option 2
If option 1 is not available or patient explicitly states, they would like to be supported by an external service.
External get healthy Rotherham service by contacting:
- Phone: 01709 718 720
- Email: gethealthyrotherham@nhs.net
14.4.3 North Lincolnshire
14.4.3.1 Option 1 (preferred)
North Lincolnshire healthy lifestyles service contact:
- Phone: 01724 298 212
- Email: healthylifestyles@nhs.net
14.4.3.2 Option 2
If option 1 is not available or patient explicitly states, they would like to be supported by an external service.
Not available.
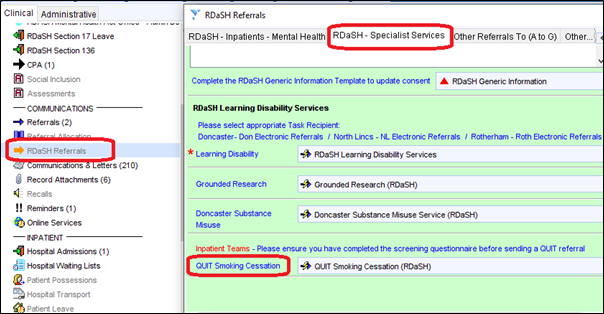
14.5 Appendix E Referral form for trust patients to the smoking cessation team
Located under “RDaSH Referrals”, “RDaSH Specialist Services”, then “QUIT Smoking Cessation”.
14.6 Appendix F Smoking risk assessment for inpatient services
14.7 Appendix G Electronic cigarettes guidance
14.7.1 National guidance
- Overview: e-cigarettes (vapes) are battery-powered devices delivering nicotine via inhaled vapor. they can be nicotine-containing or nicotine-free and are widely used as a smoking cessation aid. Public Health England (PHE) supports their use for smokers, as they are less harmful than smoking.
- Support: the NHS long term plan (2019) and care quality commission (CQC, 2018) endorse the use of e-cigarettes in mental health and learning disability services as a smoking cessation tool.
14.7.2 Health and safety of e-cigarettes
- Health impact: e-cigarettes are considered at least 95% less harmful than smoking but are not risk-free. PHE advises reporting any adverse reactions to e-cigarettes via the yellow card scheme (opens in new window).
- Exposure risk: the risk to bystanders from e-cigarette vapor is low, though those with respiratory conditions may be sensitive. Adjustments should be made as needed for comfort.
14.7.3 Types of e-cigarettes
- Cigalikes: look like traditional cigarettes; small batteries; disposable or rechargeable.
- Pod vapes: small, rechargeable with replaceable pods containing e-liquid.
- Vape pens: pen-shaped, refillable with e-liquid; often have adjustable settings.
- Box kits or mods: box-shaped devices with larger batteries and adjustable power settings.
14.7.4 E-cigarettes permitted on trust premises
14.7.4.1 Inpatients
- Offer nicotine replacement products, including disposable e-cigarettes, on admission. Authentic personal devices should be inspected and can be restricted if counterfeit
- Vaping is permitted outdoors but not indoors. Patients who are in isolation for a health reason (such as COVID-19) may not vape in their rooms and should be offered alternative NRT.
14.7.4.2 Community patients, visitors, and colleagues
- Community patients can use personal vapes outdoors and should be referred to the QUIT service. Contact quit@nhs.net for referrals.
- Visitors may use personal vapes outdoors but cannot charge them on-site.
- Colleagues may vape off-site, not in uniform or trust vehicles, they can access QUIT support at quit@nhs.net.
- Smoking paraphernalia must be stored in lockers, not on wards.
14.7.4.3 E-cigarettes and fire safety
- Risks: fires from e-cigarettes are rare but can occur due to malfunctioning lithium batteries.
- Safety measures:
- use only the designated charger
- do not leave charging devices unattended or overnight
- store batteries and chargers in a cool, dry place
- avoid charging near flammable materials or medical oxygen
- report any safety concerns to the estates team
14.7.4.4 Self-harm and ligature risks
- Risk assessment: conduct individual risk assessments for e-cigarettes to ensure safe use and storage.
- Storage: store devices centrally if there are safety concerns and supervise their use. E-liquids should be managed carefully to prevent ingestion risks.
- Charging cables: charging cables may present a ligature risk. A risk assessment should be completed for any patient who has a charging cable.
14.7.4.5 Risk assessment and general management
Checklist:
- Verify CE mark, check for damage or tampering, and ensure proper condition of devices and accessories.
- Faulty devices should be disposed of according to trust waste management policy.
- Charging should be done in designated areas, not in patient bedrooms.
Report any issues or incidents involving e-cigarettes on the IR1 system under:
- type of incident: security, loss or damage
- cause group: security, theft, loss or damage
- cause: smoking policy breach or concern
14.7.4.6 Risks associated with lithium batteries
- Swallowing: swallowing lithium batteries requires immediate medical attention. risk assessments should be undertaken for any patient who may be at risk of swallowing the battery or vape.
- Malfunction: if a battery overheats, place the device on a dry surface to discharge and contact the manufacturer.
14.8 Appendix H Smoking or tobacco use dependency calculator (Fagerstrom test)
Document control
- Version: 6.2.
- Unique reference number: 32.
- Ratified by: Clinical policies review and approval group.
- Date ratified: 12 November 2024.
- Name of originator or author: Deputy director of nursing.
- Name of responsible individual: Executive director of nursing and allied health professionals.
- Date issued: 21 November 2024.
- Review date: 30 November 2027.
- Target audience: All trust colleagues, patients and visitors.
Page last reviewed: February 25, 2025
Next review due: February 25, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.