Contents
- Aim
- Scope
- Link to overarching policy
- Procedure
- Transport options
- Action if a patient absconds or goes missing whilst on escorted leave or during planned transport arrangements
- Transportation of infectious patients
- Reporting any incidents which occur during the transportation of a patient
- Links to other associated documents
- Appendices
1 Aim
There are times when clinical colleagues working within adult and older person’s mental health and across learning disability services are required to arrange the transportation of patients for the purpose of escort or transfer. This may be due to the patient requiring a transfer to another inpatient facility, attending legal hearings, having escorted therapeutic leave, or being supported to undertake discharge preparation or therapeutic and community activities. There may also be times when clinical colleagues are responsible for organising transport arrangements for admission to an inpatient (or other) facility.
In terms of inpatient services, it is recognised that there can be an increase in the level of risk a patient poses to either themselves or others when away from the supportive environment of the ward and clinical teams. It is important therefore that transportation activities are risk assessed, and where possible planned in advance, and that systems of working are implemented proportionate to the level of risk.
Likewise in terms of community services, there may be times when clinical colleagues (working within an agreed scope of duties and role), are required to organise transport or transport patients. It is acknowledged that at such times these employees are undertaking work activities on behalf of the trust and the risks associated with this must be assessed and effectively managed and documented accordingly.
The purpose of this procedure is to set out the arrangements for when it is required for a patient to be transported or escorted by colleagues, with particular attention being paid to the assessment and proportionate management of any identified risks. The procedure will also outline the arrangements for procuring a taxi to transport a colleague when deemed appropriate to do so.
The authorisation arrangements for the booking of transport will also be outlined to ensure a standardised approach and to provide a process which finance and procurement colleagues can effectively monitor both the contractual and financial obligations for the trust.
The contents of this procedure are to be read in conjunction with both the leave for inpatients policy and guidance (including section 17) and the section 19 transfer of patients detained under the MHA 1983 to another hospital or unit procedure. Where appropriate the safer driving at work policy must also be adhered to.
2 Scope
The contents of this procedure apply to clinical colleagues working within adult and older person’s mental health and learning disability services. Please note that forensic services have their own patient escorting procedure (forensic services manual).
3 Link to overarching policy
This procedure is overarched by the admission, transfer and discharge manual
4 Procedure
In all instances of transportation of patients, whether in community services or inpatients, the same or equivalent clinical responsibilities, multi-disciplinary team (MDT) duties and patient care planning, risk assessment and risk management principles and procedures apply.
The requirements of each individual patient whilst being escorted will vary, but each escort should wherever possible be planned, and undertaken following consideration of any risks and in line with the agreed risk management plan and, where applicable, the requirements of the Mental Health Act (MHA)1983.
4.1 Risk assessment
All patients should have a clinical risk assessment prior to any transportation or escorted leave being undertaken; this will be updated to take account of any additional or increased risks of the patient absconding. Consideration also needs to be given to the length of the journey and arrangements for adequate comfort breaks.
From this risk assessment the following will be determined:
- method of transportation
- number of colleagues escorts required
- medication that may be required during the journey
- arrangements for if comfort breaks are required
- arrangements for colleagues to remain in contact, and able to summon assistance if needed, for example, by carrying a mobile phone
- any physical health care needs that should be handed over to the escorting colleagues, for example, diabetes
4.1.1 Factors that need to be considered when assessing the risk of absconding
Factors that indicate a patient is low risk of absconding:
- no recent history of attempts or threats to abscond
- no immediate identified risk to self or others
- current mental state, stable
- compliant with treatment
Factors that indicate a patient is a medium risk of absconding:
- past attempts to abscond
- an expression that they wish to leave the inpatient ward
- impulsive behaviour
- behaviour that may pose a risk to themselves or others
- fluctuating mental state
- fluctuating compliance with treatment
Factors that indicate a patient is a high risk of absconding:
- recent attempts to abscond
- assessed as posing a significant and immediate threat to themselves or others
- exhibiting acute symptoms of mental illness
- exhibiting challenging behaviour
- non-compliant with treatment
4.2 Care planning
A care plan is to be in place for all patients for any period of leave from the inpatient ward, including escorted leave. The care plan will be informed by the outcome of the risk assessment and include details of the arrangements that need to be considered as set out in section 4.1 above.
It should, where relevant also include the following:
- nature of the escorted leave
- reason escort required
- duration of leave
- destination
- transport arrangements
- number and skill mix of the colleagues undertaking the escort
- action to be taken in the event of the patient absconding
- arrangements for the administration of medication
4.2.1 Potential use of restraint
Where restraint is needed to be used to keep the person safe, it should only be carried out with:
- the person’s consent
- under the MHA 1983
- or where the person lacks capacity, in the person best interests under the Mental Capacity Act (MCA) 2005
- under common law
Where restraint is used the following conditions must be met:
- the person taking action must reasonably believe that restraint is necessary to prevent harm to the person who lacks capacity
- the amount or type of restraint used and the amount of time it lasts must be a proportionate response to the likelihood and seriousness of harm
- the use of the least restrictive option must be always considered
4.2.2 Safe transportation of patients with disabilities or mobility difficulties
As part of the assessment there should be a discussion with the patient and clinical team as to their limitations and requirements for safe and comfortable transportation. Having a physical disability or mobility difficulty does not preclude the use of a car, but in such cases a moving and handling risk assessment will be completed and consideration be given to:
- what assistance the patient will need to get in and out of the car
- the amount of legroom provided in the car
- whether there is capacity in the vehicle for a wheelchair or other equipment to be carried
4.3 Medication
Where medication is required during the escort this should wherever possible be ordered in advance. Colleagues should ensure there is sufficient supply for the journey, and it is to be carried either by one of the colleagues undertaking the escort, or in a secure area of the car for example, locking glove compartment or rear boot.
Patients are not to hold their own medication during any colleague escorted leave unless this is part of the care plan and reflected in the patient risk assessment.
4.4 Transport of clinical records with the patient
Any clinical records which are to be carried during the escort must be in an appropriate, sealed package and clearly addressed for the destination, with no patient identifiable information visible. Clinical Records are to be carried either by colleagues, or in a secure area of the vehicle. The patient must not be left unsupervised with their clinical records.
5 Transports options
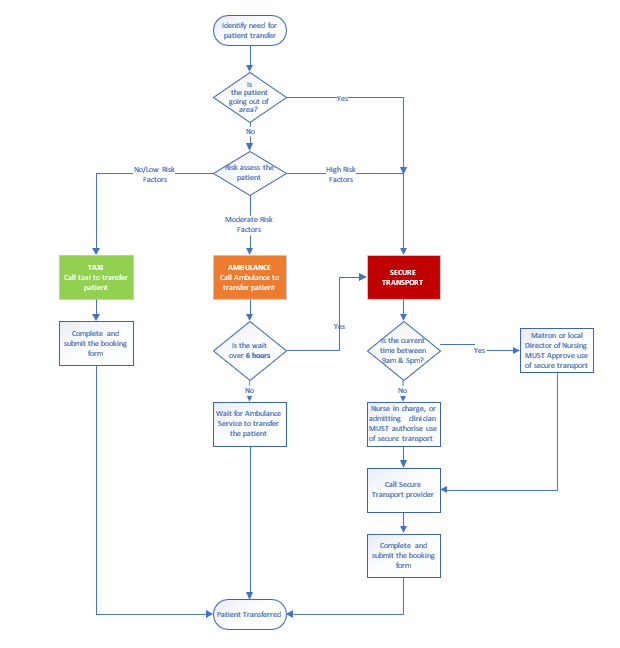
5.1 Transport options procedure
- Identify need for patient transfer.
- Is the patient going out of area?
- If yes, proceed to 5.1.1.3 secure transport.
- If no, proceed to 5.1.1 risk assessment.
5.1.1 Risk assessment
Assess the patient:
5.1.1.1 If no or low risk factors (taxi)
- Call a taxi to the transfer patient.
- Complete and submit the booking form.
- Patient transferred.
5.1.1.2 If moderate risk factors (ambulance)
- Call ambulance to transfer patient
- Is the wait over 6 hours?
- If yes, proceed to 5.1.1.3 secure transport.
- If no, wait for ambulance service to transfer the patient.
5.1.1.3 If high risk factors or going out of area (secure transport)
- Is the current time between 9am and 5pm?
- If yes, matron or local director of nursing must approve use of secure transport.
- If no, nurse in charge, or admitting clinician must authorise use of secure transport.
- Call secure transport provider.
- Complete and submit the booking form.
- Patient transferred.
5.2 Use of trust owned or colleague vehicles
A small number of colleagues, who work within an agreed scope of duties and roles will be supported to transport patients (and sometimes carers) in their own vehicles (or in equivalent work provided vehicles, such as a ward, service people carrier or car). These colleagues would ordinarily be allied health professionals or relevant team members supporting patients with rehabilitation activities in the community or transporting patients in their cars for home assessments and to progress therapy goals linked to rehab or discharge from inpatient units.
The trust has a responsibility to acknowledge the risks associated with this and these must be assessed and effectively managed.
In situations where it is agreed that colleagues can transport patients (and or carers) the team manager must be satisfied that:
- there is an overall clinical rationale
- the activity fits with the role and duties of the colleague and the colleague consents to using their vehicle for this purpose
- the use of this transportation is in line with the patient’s care plan and risk assessments or procedures are in place along with any necessary controls before the journey is undertaken
- that the necessary vehicle, and driver requirements are fulfilled in line with the safer driving at work policy and the colleague has appropriate business insurance that explicitly covers them for this purpose
- arrangements are in place in the event of breakdown, colleague illness or extreme weather
- in the case of work provided vehicles, such as unit minibus or car, that any additional driver training is completed and associated procedures are followed
The team manager should also be satisfied that the colleague has competence to:
- undertake or seek completion of necessary risk assessments that consider and accommodate the needs of the patient and any hazards of the trip, the activity, any equipment to be carried
- follow the associated patient risk management plans and be able to dynamically review situations, tasks or changes in patient needs or risks to make changes or seek additional guidance or help and make use of related procedures (such as summoning help or emergency services)
- summon emergency assistance, and have the means to do this such as, a phone
- recognise situations and scenarios that may arise with patients (and or carers) during transportation where safety could be compromised and be competent to take appropriate action
If the colleague is required to assist patients in or out of vehicles or loading and unloading, the team manager must be satisfied that:
- the colleague is up-to-date with the required level of moving and handling training and able to assist in transfers in and out of their vehicle for the client group
- the colleague is up-to-date with all other relevant risk management training completed, including infection prevention and control, managing violence and aggression, clinical risk assessment and management
- any specialist equipment or protective clothing is supplied if this is required for example, spill kits and first aid kits
If it is a three colleague escort the patient is to be seated between two staff for the duration of the journey. In the event of it being a single colleague escort for safety reasons the patient is not to be seated behind the driver. All colleagues must exit the car before opening the door for the patient, to minimise the risk of absconding.
5.3 Use of local ambulance service
- Rotherham or Doncaster, Yorkshire ambulance service
- North Lincolnshire, East Midlands ambulance service
All RDaSH inpatient wards (including the Woodlands in Rotherham) in the event of a medical emergency will call an ambulance using 222 internally.
In this situation the ward colleagues must brief the ambulance colleagues on any identified risks, and if necessary, accompany the patient in the ambulance. It is also important that the Nurse in charge contacts the local accident and emergency department to give them information as to the patient’s mental state, legal status, capacity to consent, treatment plan, and identified risks. However, if this is not possible, an accompanying letter with the information on should be sent with the ambulance or escorting colleague.
In other non-emergency situations, an ambulance may need to be arranged. Examples of these scenarios are including, but not limited to, transfer of patients between RDaSH sites, transfer from acute providers to an RDaSH site, if the patient has a disability or physical condition which makes it difficult or uncomfortable, or not possible for them to travel in a car. In these cases, a booking will be made through the ambulance call centre as far in advance as possible of the transport being required. When making the booking colleague should inform the ambulance service of any identified risks, and escort requirements (as this may influence the type of ambulance and pick up arrangements). This method of transport should be used as a primary option ahead of using private transport services where clinically possible. Colleagues need to be aware that non-urgent transfer requests may have an extended response time of 4 to 6 hours. If the response time is beyond this timescale, alternative transport options can be considered.
In community services a non-emergency ambulance may be requested to transport a patient to an inpatient setting. However, if this wait is several hours and there is a risk of impact to the patient’s mental health, if risk assessed and appropriate to do so alternative forms of transport may be used to transport the patient. This must be documented in the patient’s risk management plan (see section 4.1).
5.4 Use of taxis
There will be times when transportation of patients in a taxi is safe and appropriate. This must be risk assessed by the patient’s responsible team or ward and a taxi booked if safe and reasonable to do so.
Some examples of when use of a taxi may be appropriate are:
- attendance for a planned hospital appointment for informal patients and those patients on a section accessing section 17 leave and therefore assessed as low risk
- facilitating a patient’s home visit
- to facilitate contact with family members or carers when we have a patient out of area and there are no alternative forms of transport available
- if a patient requires urgent treatment or assessment at a general hospital, the wait time for an ambulance is excessive, and the patient is viewed by the nursing or community team as low risk and therefore conveyance by taxi will prevent further deterioration in physical healthcare
- admitting a patient to one of the crisis houses when there is no alternative transport available
- to facilitate a planned appointment with the Crisis team at one of the trust sites, this could be due to the risk associated with the patient and therefore unsuitable to have the appointment in their own home or if the patient does not have any access to other transport
- to enable a patient to access safe space or crisis cafés
- when an informal patient is being repatriated or moved to an alternative trust or NHS mental health setting
- a patient is being discharged home or utilising home leave and there is no access to appropriate public transport, or a family member is not available to transport them
- transporting perinatal patients to mother and baby units when deemed appropriate by a community team
- a patient has been assessed in accident and emergency (A and E) and does not require admission to hospital home and there is no access to appropriate public transport, or a family member is not available to transport them
- a patient is assessed in the 136 suite and does not require admission to hospital home and there is no access to appropriate public transport, or a family member is not available to transport them
Prior to transporting a physically ill patient in a taxi, a review should take place jointly by a medic and a nurse to determine the suitability of this transport option, where appropriate please refer to the guidance in the patient falls policy (prevention and management) manual. If deemed appropriate the patient must be accompanied by a colleague.
Note: There may be occasions when a taxi is required to transport a colleague. Such occasions may include:
- when additional colleagues are required at an acute general hospital to facilitate a change of observation level
- when colleagues are deployed to another hospital site, and they do not have business insurance and therefore are unable to use their own vehicle or do not have access to a vehicle
- a colleague is injured whilst on duty and requires hospital assessment or to return home and there is no alternative transport available
5.5 Use of private transport
5.5.1 Rationale for use of private transport
There may be occasions when it may be necessary to employ the services of a specialist transport and escort company.
This would ordinarily be for the transportation of any detained patient as they require a higher level of supervision or for those patients who cannot tolerate a lengthy wait (more than 2 hours) for a local ambulance.
Other examples of when private transport may be required include:
- if a patient requires urgent treatment or assessment at a general hospital and the nursing or community team feel there is a risk of the patient absconding, assaults on colleagues or self-harming behaviours
- regardless of detention: if the patient is not known to the nursing team or admitting professional and therefore a full assessment of risk cannot take place (for example a non RDaSH patient requiring transport to re-patriate them to their local area from the 136 suite or having been on the ward less than 72 hours)
- there is concern regarding the patient’s level of aggression in their community placement and therefore conveyance by an ambulance is not deemed safe by the admitting professional
- to bring a patient from the community into a mental health hospital setting if the professional feels they are at risk and unable or unwilling to make their own way in
- to transport a patient from one seclusion facility to another
- a patient is transferring to a secure unit, locked rehab placements or another specialist placement
5.5.2 Authorisation
The decision regarding transport for an in-patient will be made by the nurse in charge in discussion with the clinical team as and when necessary.
For community patients, the admitting professional will decide on the most appropriate form of transport and liaise with the relevant care group for authorisation.
If the admitting professional is non RDaSH colleague (for example external trust colleagues or local authority colleague) the request should be made to the patient flow bed manager for authorisation during working hours and the allocated care group bed manager out of hours.
5.5.3 Booking a taxi
All bookings for Doncaster taxis are to be made through the Tickhill Road Hospital main reception. The contracted taxi supplier is Drive.
All bookings for Rotherham and North Lincolnshire taxis are to be made with the contracted taxi supplier.
- Phone Rotherham, A1 Taxi’s: 01709 555555
- Phone Scunthorpe, 121 Taxi’s: 01724 355555
The person ringing to make the booking must have the details of the account number (where necessary), date, time, name of passenger, name of colleague making the booking, details of the journey and the department’s budget code for it to be charged against.
When booking a taxi, the nurse in charge or admitting professional must complete the taxi booking request form (appendix V) and forward this to:
- the service manager, modern matron or admin team (as per local agreement) for oversight and processing
5.5.4 Contacting the private transport company
The primary contractor for RDaSH is exclusive secure patient transport.
- Phone: 0843 523 6264 (select option 1)
- Online: please see link secure care services
- Email: duty.team@securecareservices.co.uk
If exclusive secure patient transport is unavailable, then the V-care Ltd may be utilised.
- Phone: 0800 5999161, out of hours use 07704146871
- Online: please see link V care (opens in new window).
- Email: robert.thomson@vcare24.co.uk
When making the booking it must be made clear to the company the purpose of the transport request and a full and robust handover of risk and patient care plans shared.
The transport company will request the following information:
- NHS number
- patient’s home address
- patient details:
- age
- height
- weight
- build
- illness and mental health section (if applicable)
- medical conditions
- history of violence, aggression or assault
- current behaviour and trigger factors
- history of absconsion and current risk
- history of self-harm and current risk
- full details of the person authorising payment of transfer
- handcuff authorisation (if applicable)
- details of any medication administered
When requesting private transport, the nurse in charge or admitting professional must complete the private transport request form (appendix W) for oversight and processing and forward this to:
- the service manager or modern matron
- the secure transport company: for exclusive secure transport remittance@securecareservices.co.uk or for V care finance@vcare24.co.uk.
- the relevant finance manager for the care group
5.5.5 Payment of invoices
All invoices for payment will be directed in the first instance to the purchase ledger department via email rdash.purchaseledger@nhs.net so that the invoice can be registered on the system. It will then be coded to the correct budget and forwarded onto to the locality manager within the relevant care group for authorisation so it can be processing for payment or recharged to the organisation who has agreed to pay.
Colleagues should be clear as to who will be paying for the invoice, and this will depend on the named integrated care board (ICB) for the patient. Where any agreement to recharge has been made this information should be forwarded onto to the relevant finance lead for the care group.
Patients who are registered with a general practitioner (GP) in Doncaster, Rotherham or North Lincolnshire who need to be conveyed to a hospital out of area will be paid for by their responsible ICB. This may be covered in the block contract arrangements the trust has with each ICB and would be reviewed on a case by case basis between finance and the contracting team, and any recharging discussed and agreed with the commissioner.
Note, in the first instance, all invoices will be paid by RDaSH and on some occasions this can then be recharged to the appropriate provider or ICB providing authorisation has been sought in advance. It is therefore imperative that all the necessary information is provided on the transport request form (appendix W). This will enable the finance team to be able to recharge an alternative provider or ICB where necessary within the allocated timeframe (as per the Who pays? guidance, which is 30 days). If this is not provided and the trust cannot recharge the other provider or ICB within the timeframe, then the cost of the transport will come out of the ward or service’s budget who that requested it.
Where the cost of the transport is to be met by the trust, the budget code and purchase order (where known) should be provided on the transport request form. If this information is not readily available, the nurse in charge or admitting professional should detail the name of the service or ward.
5.6 Request for police assistance
As the patient is under the care of RDaSH, the police have no authority under which to transport our patients, so colleagues should not routinely contact them for assistance.
The exceptions to this are:
- the transfer of a patient detained on a section 136 to another place of safety. The police have their own policy on transferring a patient on a section 136 and 135
- the return of a patient detained under the MHA who has absconded
- if a patient is arrested
5.7 Escorting a patient to court
If a detained inpatient is to be escorted to court, colleagues are to remain with them even if they are to be held in the cells.
In the case of a patient being held in the cells the accompanying colleagues will remain outside of cells in the main court waiting area ensuring that any key risk information is communicated to the court custody team and an agreement made in relation to the safe management of the patient whilst in the holding cells.
6 Action if a patient absconds or goes missing whilst on escorted leave or during planned transport arrangements
Whilst all practical steps should be taken when escorting, colleagues must never put either their own safety or that of others at risk in taking measures to prevent patients from absconding.
If practical to do so a search of the immediate area should be undertaken by the escort, and if the patient is not located, the ward will be contacted by the escort, and notified of the absconding.
The nurse in charge of the ward will then implement the relevant actions from the trust patients missing or absent without leave (AWOL) policy. If the patient is located but the escorting colleagues have concerns about their ability to retake the patient safely, assistance should be sought from the police.
Where a patient in the community absconds or goes missing during planned transport arrangements, it is expected that the community professional responsible for the patient will also implement the relevant actions from the trust patients missing or absent without leave (AWOL) policy.
7 Transportation of infectious patients
Movement of infectious or potentially infectious patients must be kept to a minimum. When it is necessary to transport patients to other wards, departments or premises, precautions taken to minimise the risks of transmission must continue. If it is possible to delay an investigation or transfer without adversely affecting the patient’s clinical management this should be considered. However, the presence of an infectious disease should not delay urgent clinical investigations. The receiving area or transport team must be informed prior to transfer to ensure that they have the necessary precautions in place and that appropriate facilities are available. Where patients with known or suspected infections are being transferred for appointments, they should be seen at the end of the list and not left in waiting areas. This will allow adequate cleaning of the environment and equipment following the appointment and reduce the risks of transmission to other patients. Please refer to the infection prevention and control manual for further guidance relating to specific infections and precautions required. Consult the IPCT for any further advice or guidance.
8 Reporting any incidents which occur during the transportation of a patient
Any incidents which occur during an escort (including absconding) are to be reported at the earliest opportunity onto the electronic incident reporting system via the trusts safeguard electronic incident reporting system and the responsible clinician notified.
9 Links to other associated documents
This protocol does not stand in isolation but is to be used in conjunction with the trusts’ health and safety policies, including:
- Safer driving at work policy
- Leave for inpatients policy and guidance (including S17)
- Section 19 transfer of patients detained under the MHA 1983 to another hospital or unit procedure
- Patients missing or absent without leave (AWOL) policy
- Patient escorting procedure (forensic services manual)
- Police assistance and conveyance for the admission of patients detained under MHA 1983 to hospital
- Infection prevention and control manual
- Patient falls (prevention and management) policy
10 Appendices
Please see admission, transfer and discharge manual including patient flow and out of hours (OOH) procedures webpage for appendices attached to this procedure.
- Appendix V taxi booking form
- Appendix W private ambulance or secure transport booking form
Document control
- Version: 6.
- Unique reference number: 403.
- Date ratified: 7 June 2024.
- Ratified by: Operations management CLE group.
- Name of originator: Head of patient flow.
- Name of responsible individual: Chief operating officer.
- Date issued: 1 August 2024.
- Review date: 31 August 2027.
- Target audience: Mental health and learning disability clinical colleagues.
- Description of change:
- added a flowchart to visually aid decision-making
- moved the section on the use of ambulances earlier in the policy to support the flowchart instructions to use ambulances
- updated the booking form to add in waiting for ambulance response
- change of period for acceptable wait for ambulance response.
- grammar and spelling corrections
- updated job titles to reflect the new organisation structure
Page last reviewed: November 15, 2024
Next review due: November 15, 2025
Problem with this page?
Please tell us about any problems you have found with this web page.