Contents
1 Introduction
The decision and procedure to resuscitate, or not when there is a valid do not attempt cardio-pulmonary resuscitation (DNACPR) decision in place for both adults and children within RDASH are all in one manual. The introduction of, and rationale for, each procedure will be within the relevant chapter.
2 Purpose
The purpose of this manual and the linked procedure documents is to provide clear, concise guidance on managing, for both adults and children:
- the risks associated with resuscitation
- the systems in place to support effective resuscitation provision
- the deteriorating patient
- DNACPR decision
- recommended summary plan for emergency care and treatment (ReSPECT)
The manual outlines the duties and responsibilities of the trust to comply with the relevant local and national legislation and guidance and monitor compliance with this manual so that an effective service is provided.
3 Scope
This manual applies to all managers with responsibilities derived from it, and all staff (clinical and non-clinical), including bank, agency and temporary staff who may need to summon help if they come in to contact with a patient, visitor or member of staff who becomes acutely unwell.
4 Responsibilities, accountabilities and duties
4.1 Chief executive
The chief executive is responsible for making arrangements to support the safe and effective implementation, monitoring and review of this policy manual.
4.2 Medical director and chief operating officer
These directors are responsible for implementation and monitoring of the policy manual within their areas of responsibility.
4.3 Consultants and medical officers
Consultants and medical officers in charge of patients’ care retain overall responsibility for the decisions relating to procedures within this policy manual.
4.4 Resuscitation committee
The resuscitation committee are responsible for reviewing the trust’s assurance processes within this policy manual and to oversee the annual audit work plan adhering to the UK Resuscitation Council Quality Standards (see appendix A).
4.5 Resuscitation service
- Liaise with managers or modern matrons to formulate suitable staff training programmes to support effective implementation of this policy manual.
- Deliver training using the current national guidelines.
- Maintain a central record of training delivered and produce reports on training compliance.
- Discuss with the managers or modern matrons the approach to be taken with staff who do not successfully complete the training assessments.
- Act as specialist advisors to the trust on resuscitation and related matters.
- Produce an annual audit of resuscitation events, resuscitation equipment, choking incidents and DNACPR or ReSPECT orders
- Produce a quarterly audit report on the continual availability of equipment, see appendix D, emergency equipment required in healthcare areas.
- Facilitate policy and practice development and organisational learning as a result of audit.
- Support Managers in facilitating an environment where incidents are reviewed in an open and positive manner, involving staff at all levels in improving practice and promoting organisational learning
- Be available as a source of specialist advice and support to managers and staff, including incident debriefing.
- Represent the trust on the regional DNACPR working party and the Doncaster locality End of Life group as the DNACPR lead for the trust.
- Lead the review and updating of this policy.
4.6 Managers or modern matrons
- Disseminate, implement and monitor implementation of this policy manual within areas of responsibility.
- Facilitate, support and monitor ward or team managers in their responsibilities with regard to policy implementation and monitoring.
- Identify and allocate resources in order to comply with this policy manual.
- Make available appropriate and suitably maintained resuscitation equipment, maintaining up-to-date medical devices inventories in all areas of responsibility.
- Promote incident reporting and audit requirements as specified within the policy through local induction processes in all areas of responsibility.
- Facilitate an environment where incidents are reviewed in an open and positive manner, involving staff at all levels in improving practice and promoting organisational learning.
- Proactively seek advice and support from the resuscitation service.
4.7 Ward or team managers
- Facilitate effective local induction processes for all new starters
- Manage the process of releasing staff for training and updating at least annually in the skills relevant for their area, in line with the mandatory risk management training policy.
- Maintain staff training records for the area, including temporary, bank and agency staff.
- Proactively identify risks due to lack of training or resources to the manager or modern matron.
- Manage and maintain the resuscitation equipment within the area of responsibility via:
- an up-to-date medical devices Inventory
- signed and dated daily and weekly equipment check records (as per requirements set out in appendix D continual availability of equipment, see appendix D, emergency equipment required in healthcare areas), in line with the manufacturer’s recommendations. A record of these checks will be kept for 3 years
- report any equipment issues immediately to the manager or modern matron
- adequate stocks of disposable or single use parts of the resuscitation equipment required in that area, such as pocket masks, oxygen masks, airway tubes, defibrillator pads etc. to maintain continued functioning of the equipment by immediate replacement
- Maintain the equipment ready and available for use for another event as soon as practicable after a resuscitation attempt where the equipment is used.
- Make timely arrangements for staff involved in a resuscitation event to be supported, debriefed, and offered counselling as required in conjunction with the resuscitation officer.
- Facilitate an environment where incidents are reviewed in an open and positive manner, involving staff at all levels in developing policy and practice and promoting organisational learning.
- Proactively seek advice and support from resuscitation service.
4.8 Clinical and non-clinical staff
- Adhere and implement this policy manual within the scope of their job role (the resuscitation council expects all staff to recognise cardiac arrest, to commence cardio-pulmonary resuscitation (CPR) and call for help).
- Report any issues which affect the effective implementation of this manual to their manager, for example, access to training or equipment.
- Report all incidents as per the incident reporting policy including the use of the appropriate cardiac arrest report form.
- Maintain a personal record of their own training.
- Contribute to the review of incidents in an open and positive manner in order to improve practice and promote organisational learning.
5 Procedure or implementation
- Resuscitation and the deteriorating adult procedure
- Do not attempt cardiopulmonary resuscitation (DNACPR) adult
- Do not attempt cardiopulmonary resuscitation (DNACPR) child
- Recommended summary plan for emergency care and treatment (ReSPECT)
6 Training implications
In adherence with the expectations of the Resuscitation Council UK, all staff should have basic knowledge and skills in resuscitation. All staff should be equipped to recognise cardiac arrest, to commence CPR and call for help. All staff should attend, as a minimum, community life support (CLS) every 12 months.
All registered nurses, doctors, and nursing assistants working in areas where physical restraint, rapid tranquilisation or seclusion may be required, will be trained to a level equal to the immediate life support (ILS) course of the Resuscitation council UK. This will be repeated every 12 months.
All registered nurses and nursing assistants working within areas with immediate access to a defibrillator will be trained to the equal level of the immediate life support course of the Resuscitation Council UK. This will be repeated every 12 months.
When practicable and appropriate, the training will be contextual, and scenario based. Staff who do not successfully complete the training assessments will be recalled within 1 month for further training. Failure to complete the assessments after 3 attempts will be discussed with the manager by the resuscitation service.
Basic training on DNACPR and ReSPECT will be within the CLS and ILS sessions. For clinicians who have such discussions within their job roles (includes some specialist nurses identified in the resuscitation committee), additional training is required (see DNACPR and ReSPECT sections)
The Yorkshire and Humber e-learning is an excellent source of information and can be used as a training resource in team meetings etc. It can also be used as an individual training resource and can be found on the trust eLearning platform.
6.1 All non-clinical and community clinical staff community life support training (includes do not attempt cardio-pulmonary resuscitation (DNACPR) or recommended summary plan for emergency care and treatment (ReSPECT))
- How often should this be undertaken: 12 months.
- Length of training: 3 hours.
- Delivery method: Face to face.
- Training delivered by whom: Resuscitation service.
- Where are the records of attendance held: Electronic staff record (ESR).
6.2 All in-patient clinical staff immediate life support (ILS) training
- How often should this be undertaken: 12 months.
- Length of training: 3 hours.
- Delivery method: Face to face.
- Training delivered by whom: Resuscitation service.
- Where are the records of attendance held: Electronic staff record (ESR).
6.3 Clinicians that have escalation plan discussions in care groups that have recommended summary plan for emergency care and treatment (ReSPECT), e-learning
- How often should this be undertaken: One-off
- Length of training: 40 minutes
- Delivery method: E-learning, ReSPECT (opens in new window)
- Training delivered by whom: Resuscitation Council UK
- Where are the records of attendance held: Electronic staff record (ESR).
6.4 Clinicians that have escalation plan discussions in care groups that have recommended summary plan for emergency care and treatment (ReSPECT)
- How often should this be undertaken: One off and more if required.
- Length of training: 1 hour.
- Delivery method: Face to face clinical supervision for additional sessions.
- Training delivered by whom: Nurse consultant in palliative care. consultants in older peoples mental health.
- Where are the records of attendance held: Electronic staff record (ESR).
6.5 For care groups that do not have the recommended summary plan for emergency care and treatment (ReSPECT) document
Clinician completing DNACPR decisions, see link above.
- How often should this be undertaken: One off.
- Length of training: 1 hour.
- Delivery method: E-learning.
- Where are the records of attendance held: Electronic staff record (ESR).
As a trust policy, all staff need to be aware of the key points that the policy covers. Staff can be made aware through a variety of means such as:
- all user emails for urgent messages
- one to one meetings or supervision
- continuous professional development sessions
- posters
- daily email (sent Monday to Friday)
- practice development days
- group supervision
- special meetings
- intranet
- team meetings
- local induction
7 Monitoring arrangements
7.1 Policy implementation
- Policy implementation including:
- requirement for a documented plan for vital signs monitoring that identifies which variables need to be measured, including the frequency of measurement
- use of an early warning system within the trust to recognise patients at risk of deterioration
- actions to be taken to minimise or prevent further deterioration in patients
- how the trust documents that resuscitation equipment is checked, stocked and fit for use
- incident reports of resuscitation events
- incident reports of choking situation events
- staff training, as identified in the training needs analysis
- How: Resuscitation audit.
- Who by: Resuscitation officer.
- Reported to: Quarterly and annually.
- Frequency: Resuscitation committee.
8 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
8.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
8.1.1 How this will be met
There are no additional requirements in relation to privacy, dignity and respect.
8.2 Mental Capacity Act (2005)
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals’ capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act (2005) (section 1).
9 Links to any other associated documents
- Consent to care and treatment policy
- Clinical risk assessment and management policy
- Clinical skills policy
- Incident management policy
- Infection prevention and control
- Mandatory and statutory training policy
- Mental Capacity Act (2005) policy
- Medical devices management policy
- Slips, trips and falls for staff and visitors, prevention and management policy
- Rapid tranquillisation policy and guidelines (pharmacological management of violence)
10 References
- Resuscitation Council (UK) (2021) resuscitation guidelines (opens in new window).
- Guidance, DNACPR and CPR decisions (opens in new window).
- ReSPECT, Resuscitation Council UK (opens in new window).
- Mental Capacity Act (2005) (legislation.gov.uk) (opens in new window).
- Advance decisions to refuse treatment guide (england.nhs.uk) (opens in new window).
- Advance care planning, end of life care, Royal College of Nursing (rcn.org.uk) (opens in new window).
11 Appendices
11.1 Appendix A Resuscitation committee terms of reference
11.1.1 Name of committee or group
Resuscitation committee.
11.1.2 Purpose
The purpose of this resuscitation committee is to review the trust’s assurance processes for resuscitation and to oversee the annual audit work plan taking into account UK Resuscitation Council Quality Standards.
11.1.3 Membership
The membership of the group would include:
- medical director (chair)
- nurse consultant, St John’s Hospice (deputy chair)
- lead learning and development facilitator, mandatory and statutory training
- chief pharmacist or a nominated deputy
- head of patient safety
- clinical representation from each care group as determined by the relevant associate nurse director
- medical representative
- allied health professional representative
- patient governor representative
- non-executive director
11.1.4 Attendance
All members, or a nominated deputy, from each care group should attend each meeting. Each care group representative should have a clinical background. In addition, other directors, senior managers and advisors will be invited to attend as and when required. Attendance will be recorded in the minutes of each meeting.
11.1.5 Quoracy
The chair or deputy chair and a clinical representative from each care group should be present. The senior clinical representative will be determined by the associate nurse director from each care group.
11.1.6 Meeting arrangements (frequency, chair, venue, administrative support arrangements)
Meetings shall be held 3 monthly. Administrative support will be provided by the executive medical director’s personal assistant.
11.1.7 Key responsibilities or objectives or duties or powers
These key responsibilities (KR) will be represented in the agenda responsibilities of the resuscitation committee as defined by the Resuscitation Council (UK) include:
- KR 1, ensuring implementation and adherence to national resuscitation guidelines and standards
- KR 2, defining the role and composition of the resuscitation team
- KR 3, ensuring that resuscitation equipment for clinical use is available and ready for use
- KR 4, ensuring that appropriate resuscitation drugs (including those for peri-arrest situations) are available and ready for use
- KR 5, planning adequate provision of training in resuscitation
- KR 6, determining requirements for and choice of resuscitation training equipment
- KR 7, preparing and implementing policies relating to resuscitation and treatment of anaphylaxis
- KR 8, preparing and implementing policies relating to prevention of cardiac arrest
- KR 9, preparing and implementing a policy on resuscitation decisions, (for example, DNACPR decisions), and advance care planning (this is usually in collaboration with palliative care teams)
- KR 10, quality improvement, action plans based on audits, for example, review of audit data using National Cardiac Arrest Audit data for benchmarking
- KR 11, recording and reporting of patient safety incidents in relation to resuscitation
- KR 12, the resuscitation committee is responsible for implementing operational policies governing cardiopulmonary resuscitation, practice and training
An annual audit report will provide assurance against each of the above key responsibility areas and will include relevant audit data.
11.1.8 Receipt of minutes and reports from
Completed resuscitation audits and any other relevant clinical audits undertaken.
11.1.9 reporting arrangements
Quality Committee for assurance in relation to the key responsibilities outlined in section 7 via an annual resuscitation report.
Safety and quality operational group.
The Executive Management team for any issues that require an urgent executive operational response.
Involvement of a designated non-executive director will have oversight of, and will sit as part of, the resuscitation committee.
11.1.10 Date
Each year.
11.1.11 Review date
Each year.
11.1.12 Document owner or responsibility for review (lead director)
Executive medical director.
11.2 Appendix B The deteriorating patient
11.2.1 Appendix B1 New head injury flow chart
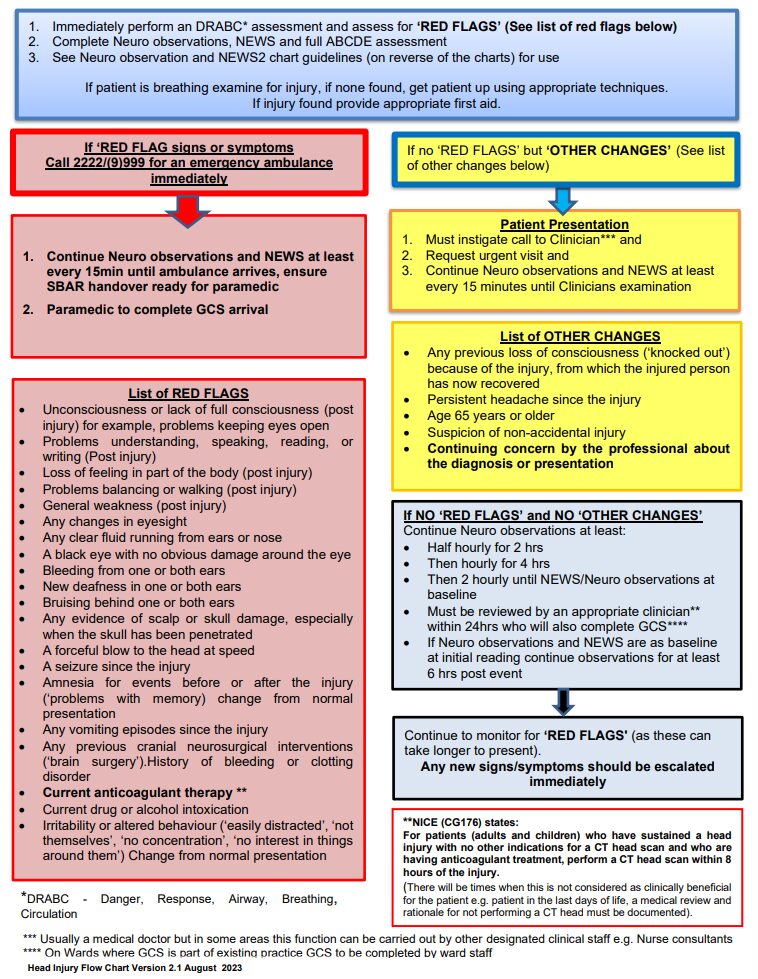
- Immediately perform an DRABC (danger, response, airway, breathing, circulation) assessment and assess for red flags (see list of red flags below).
- Complete neuro observations, NEWS and full ABCDE assessment.
- See neuro observation and NEWS2 chart guidelines (on reverse of the charts) for use.
If patient is breathing examine for injury, if none found, get patient up using appropriate techniques.
If injury found provide appropriate first aid.
11.2.1.1 If red flag signs or symptoms
If red flags signs or symptoms call 2222 or (9)999 for an emergency ambulance immediately.
- Continue neuro observations and NEWS at least every 15 minutes until ambulance arrives, ensure SBAR handover ready for paramedic.
- Paramedic to complete GCS arrival.
11.2.1.1.1 List of red flags
- Unconsciousness or lack of full consciousness (post injury) for example, problems keeping eyes open.
- Problems understanding, speaking, reading, or writing (post injury).
- Loss of feeling in part of the body (post injury).
- Problems balancing or walking (post injury).
- General weakness (post injury).
- Any changes in eyesight.
- Any clear fluid running from ears or nose.
- A black eye with no obvious damage around the eye.
- Bleeding from one or both ears.
- New deafness in one or both ears.
- Bruising behind one or both ears.
- Any evidence of scalp or skull damage, especially when the skull has been penetrated.
- A forceful blow to the head at speed.
- A seizure since the injury.
- Amnesia for events before or after the injury (problems with memory) change from normal presentation.
- Any vomiting episodes since the injury.
- Any previous cranial neurosurgical interventions (brain surgery), history of bleeding or clotting disorder.
- Current anticoagulant therapy (NICE (CG176) states for patients (adults and children) who have sustained a head injury with no other indications for a CT head scan and who are having anticoagulant treatment, perform a CT head scan within 8 hours of the injury (there will be times when this is not considered as clinically beneficial for the patient, for example, patient in the last days of life, a medical review and rationale for not performing a CT head must be documented)).
- Current drug or alcohol intoxication.
- Irritability or altered behaviour (easily distracted, not themselves, no concentration, no interest in things around them) change from normal presentation.
11.2.1.2 If no red flags but other changes
If no red flags but other changes (see list of other changes below)
11.2.1.2.1 Patient presentation
- Must instigate call to clinician (usually a medical doctor but in some areas this function can be carried out by other designated clinical staff, for example, nurse consultants).
- Request urgent visit.
- Continue neuro observations and NEWS at least every 15 minutes until clinicians examination.
11.2.1.2.2 List of other changes
- Any previous loss of consciousness (‘knocked out’) because of the injury, from which the injured person has now recovered.
- Persistent headache since the injury.
- Age 65 years or older.
- Suspicion of non-accidental injury.
- Continuing concern by the professional about the diagnosis or presentation.
11.2.1.2.3 If no red flags and no other changes
Continue neuro observations at least:
- half hourly for 2 hrs
- then hourly for 4 hrs
- then 2 hourly until NEWS or neuro observations at baseline
- must be reviewed by an appropriate clinician (NICE (CG176) states for patients (adults and children) who have sustained a head injury with no other indications for a CT head scan and who are having anticoagulant treatment, perform a CT head scan within 8 hours of the injury (there will be times when this is not considered as clinically beneficial for the patient, for example, patient in the last days of life, a medical review and rationale for not performing a CT head must be documented))
- within 24 hours who will also complete GCS (on wards where GCS is part of existing practice GCS to be completed by ward staff)
- if neuro observations and NEWS are as baseline at initial reading continue observations for at least 6 hrs post event
Continue to monitor for red flags (as these can take longer to present).
Any new signs or symptoms should be escalated immediately.
11.2.2 Appendix B2 Ligature flow chart

- Ligature found around a patient’s neck, call for help (use walkie talkie or activate alarm if available).
- Request emergency equipment and ligature cutter.
- Assess, approach patient from the front when safe to do so.
11.2.2.1 Suspected strangulation
11.2.2.1.1 Complete, body suspended by ligature from a fixed point
- Hold patient at thighs or hips and raise slightly to reduce tension on ligature.
- After tension on ligature is reduced and with assistance to support weight of patient, safely remove or cut ligature between anchor point and knot. Lay patient supine and cut ligature from neck.
- Qualified nurse to assess, perform DRABC assessment, assess for “RED FLAGS” (see list of red flags below) and undertake full set of neuro observations and NEWS2. Protect c-spine and use jaw thrust to open airway if airway is compromised.
11.2.2.1.2 Incomplete, body is not suspended entirely via a ligature
- Hold patient at torso and raise slightly to reduce tension on ligature.
- After tension on ligature is reduced and with assistance to support weight of patient, safely remove or cut ligature between anchor point and knot. Lay patient supine and cut ligature from neck.
- Qualified nurse to assess, perform DRABC assessment, assess for “RED FLAGS” (see list of red flags below) and undertake full set of neuro observations and NEWS2. Protect c-spine and use jaw thrust to open airway if airway is compromised.
11.2.2.2 Lying strangulation (body is on the floor at low level anchor point)
Slide patient up towards ligature to reduce tension and safely remove or cut ligature.
Qualified nurse to assess, perform DRABC assessment, assess for “RED FLAGS” (see list of red flags below) and undertake full set of neuro observations and NEWS2. Protect c-spine and use jaw thrust to open airway if airway is compromised.
11.2.2.3 Unsuspended strangulation
If torso is not under any ligature pressure, continue to safely remove or cut ligature.
Qualified nurse to assess, perform DRABC assessment, assess for “RED FLAGS” (see list of red flags below) and undertake full set of neuro observations and NEWS2. Protect c-spine and use jaw thrust to open airway if airway is compromised.
11.2.2.4 Red flags
- Resuscitation required.
- Suspected neck fracture.
- Difficulty or painful swallowing.
- Crepitus or subcutaneous crepitus (air under skin with crackling or crunchy feeling to touch).
- Tenderness over hyoid bone.
- Any loss of consciousness.
- Deeply indented ligature mark.
- A long period of ligature Cyanosis (blue lips and skin) not subsiding immediately after ligature removal.
- Sweating or clamminess.
- Continued coughing.
- Petechial haemorrhages (small red marks with pinpoint centres on eyes, face, neck or lips).
- Suffocation when sticking out tongue.
- Persistent breathlessness or hoarseness since ligature incident.
Call ambulance for transfer to accident and emergency or emergency department or urgent and emergency care centre
11.2.2.5 No red flags
11.2.2.5.1 National early warning score 2 (NEWS2) above baseline or any other concern
Call doctor or other designated clinician (ANP, ACP, physician associate).
Clinician review within 2 hours to undertake history and physical examination including assessment of:
- patency of airway
- breathing
- swallowing
- neurological system
Reassess for red flags. Review frequency and duration of ongoing physical observations
11.2.2.5.2 National early warning score 2 (NEWS2) at baseline and no other concerns
Monitor:
- neuro observations and national early warning score 2 (NEWS2)
- every 15 minutes for 1 hour
- every 20 minutes for next
- 3 hours (minimum)
Over next 36 hours, be alert for the emergence of:
- confusion
- sweating
- tender larynx
- mild cough
- wheezing hypoxia
- Swelling of the neck
- rapid breathing or shortness of breath
- muffled or hoarse voice
- fast and, or irregular pulse rate
- motor or sensory loss
Seek medical review if signs emerge or as indicated by NEWS2 or neuro observations.
11.2.3 Appendix B3 Normal parameter exception care plan
11.3 Appendix C Emergency drugs
11.4 Appendix D Emergency equipment
11.4.1 Appendix D1 Equipment checklist
11.4.2 Appendix D2 Equipment checklist
11.5 Appendix E Cardiac arrest report form
11.6 Appendix F Young people aged 16 and 17 years special considerations
Some special considerations apply where patients are aged 16 or 17 years.
11.6.1 Current practice relating to young persons
The Association for Children’s Palliative Care (2004) recommends that every young person with a life limiting condition should be helped, with their family, to decide on an end of life or palliative care plan.
Within RDASH, the large majority of children (16 to 18 years) needing palliative care are under specialists in Sheffield.
11.6.2 Who should or could initiate discussion, and when?
It can be appropriate for professionals looking after young people with life limiting or life threatening conditions to initiate discussion about end of life planning well before the young person is terminally ill. It may also be appropriate to begin discussions if a young person has an acute illness or repeated illness as a result of which it becomes clearer to professionals and, or the parents that the young person is moving into a terminal phase of their illness, or that they are at an increased risk of a more sudden life threatening illness or event. Usually the most appropriate professional to initiate this discussion is the named paediatrician or palliative care practitioner.
If professionals initiate discussion, consideration should be given to the sensitive timing of this and further support for the family and young person may be necessary. Decision-making should not be forced on a young person or family. If a professional initiates a discussion about do not attempt cardio pulmonary resuscitation (DNACPR) and the young person or family indicate they do not wish to continue, their wishes should be respected, and the details recorded in the young person’s medical record.
Discussion may also be initiated by the young person or family at any time.
11.6.3 Who can make decisions?
The Department of Health (2009) state that:
- ‘by virtue of section 8 of the Family Law Reform Act 1969, young people aged 16 and 17 are presumed to be capable of consenting to their own medical treatment. As for adults, consent will be valid only if it is given voluntarily by an appropriately informed young person capable of consenting to the particular intervention. However, unlike adults, the refusal of a competent person aged 16 to 17 may in certain circumstances be overridden by either a person with parental responsibility or a court’
In exceptional circumstances it may be impossible for all concerned to reach a united decision regarding the best interest of the young person. If this cannot be resolved by the patient’s consultant, the consultant should request further advice from regional experts, trust medical director and trust legal services department.
To establish whether a young person aged 16 or 17 has the requisite capacity to consent to the proposed intervention, the same criteria should be used as for adults. If a young person lacks capacity to consent because of an impairment of, or a disturbance in the functioning of, the mind or brain then the Mental Capacity Act (2005) will apply in the same way as it does to those who are 18 and over (Department of Health (2009)).
Where a young person lacks capacity to decide, a person with parental responsibility for the young person may make a DNACPR decision where they consider that to be in the young person’s best interests.
If a 16 or 17 year-old is capable of making an informed decision then it is not legally necessary to obtain additional consent from a person with parental responsibility. It is, however, good practice to involve the young person’s family in the decision-making process, unless the young person specifically wishes to exclude them, if the young person consents to their information being shared.
If a young person decides that he or she does not wish to be resuscitated and that the family should not be involved with or informed about the decision this must be urgently referred to the trust medical director and legal services department.
11.6.4 What is, and who has, parental responsibility?
Parental responsibility is defined by section 3 of the 1989 Children Act as “all rights, duties, powers, responsibilities and authority which by law a parent of a child has in relation to a child and his property”. Parental responsibility is therefore concerned with bringing the child up, caring for him and making decisions about him, including the right to consent or withhold consent for medical treatment. Parental responsibility is relinquished on a young person’s eighteenth birthday.
The Children Act 1989 sets out persons who may have parental responsibility. These include:
- the child’s mother
- the child’s father, if he was married to the mother at the time of birth
- unmarried fathers, who can acquire parental responsibility in several different ways:
- for children born before 1 December 2003, unmarried fathers will have parental responsibility if they:
- marry the mother of their child or obtain a parental responsibility order from the court
- register a parental responsibility agreement with the court or by an application to court
- for children born after 1 December 2003, unmarried fathers will have parental responsibility if they:
- register the child’s birth jointly with the mother at the time of birth
- re-register the birth if they are the natural father
- marry the mother of their child or obtain a parental responsibility order from the court
- register with the court for parental responsibility
- the child’s legally appointed guardian
- a person in whose favour the court has made a residence order concerning the child
- a local authority designated in a care order in respect of the child
- a local authority or other authorised person who holds an emergency protection order in respect of the child.
- it should be noted that:
- if a child is in local authority care parents can share parent responsibility with the local authority, this is lost if the child is adopted
- parental responsibility can also be restricted by a court order
- foster parents do not automatically have parental responsibility
- for children born before 1 December 2003, unmarried fathers will have parental responsibility if they:
11.6.5 Children in local authority care
Where a child is in the care of the local authority the child’s social worker must be involved in all of the discussions as well as parents, as the local authority shares parental responsibility with the parents. However, when a child is in voluntary care (section 20, Children Act 1989) the parents retain full parental responsibility.
11.6.5.1 What happens when a young person and a person with parental responsibility disagree about a DNACPR decision?
Decision-making with young people may be a matter of negotiation between the child, those with parental responsibility and clinicians. Inevitably there will be times when young people and those with parental responsibility for them do not agree about whether a DNACPR decision should be made.
If a young person is deemed to have the capacity to make a DNACPR decision (or believes he or she has capacity to make a decision?) and there is disagreement between the patient and those with parental responsibility despite attempts to reach agreement, legal advice should be sought.
What happens when medical staff and a young person or persons with parental responsibility disagree about a DNACPR decision?
Where medical staff are strongly of the opinion that cardiopulmonary resuscitation should not be attempted but the young person or people with parental responsibility disagree, or vice versa, a legal opinion should be sought.
11.6.6 Safeguarding issues
Where there is doubt about whether a person with parental responsibility is acting in the interest of the young person, then local safeguarding children board procedures must be instigated.
11.6.7 Education establishments
Potentially a young person may wish to continue at school with an agreed DNACPR decision in place. This can potentially cause anxieties for both the family and staff supporting that young person. Advice can be sought from a palliative care practitioner in dealing with those anxieties and what measures can be put in place to support the child and family during this period.
11.6.8 Interface with the child death overview process
Each safeguarding board has a designated paediatrician for all unexpected child deaths who are supported by a Rapid Response team. All deaths of a person under 18 years of age must be reported to the rapid response professional in the local area, who will notify the child death overview panel of the local safeguarding children board in accordance with the statutory guidance in chapter 7, Working Together to Safeguard Children 2010. DNACPR status must be reported at this time. The rapid response team contact details can be found on the local safeguarding children’s board website.
11.7 Appendix G Cardio-pulmonary resuscitation decision-making framework
- Is cardiac or respiratory arrest a clear possibility?
- no, it is not necessary to discuss CPR with the patient unless they express a wish to discuss it
- Yes, is there a realistic change that CPR could be successful?
- no, if a DNACPR decision is made on clear clinical grounds that CPR would not be successful there should be a presumption in favour of informing the patient of the decision and explaining the reason for it (see section 5). Subject to appropriate respect for confidentiality those close to the patient should also be informed and offered an explanation
- where the patient lacks capacity and has a welfare attorney or court-appointed deputy or guardian, this representative should be informed of the decision not to attempt CPR and the reasons for it as part of the ongoing discussion about the patient’s re (see section 5)
- if the decision is not accepted by the patient, their representative or those close to them, a second opinion should be offered
- Yes, does the patient lack capacity and have an advance decision specifically refusing CPR or have an appointed attorney, deputy or guardian?
- yes, if a patient has made an advance decision refusing CPR, and the criteria for applicability and validity are met, this must be respected.
- if an attorney, deputy or guardian has been appointed they should be consulted (see sections 9.1 and 10)
- No, does the patient lack capacity?
- yes, discussion with those close to the patient must be used to guide a decision in the patient’s best interests (see section 10). When the patient is a child or young person, those with parental responsibility should be involved in the decision where appropriate, unless the child objects (see section 11)
- No, is the patient willing to discuss his or her wishes regarding CPR?
- no, respect and document their wishes (see section 6.3). Discussion with those close to the patient may be used to guide a decision in the patient’s best interests, unless confidentiality restrictions prevent this
- Yes, the patient must be involved in deciding whether CPR will be attempted in event of cardiorespiratory arrest.
- If cardiorespiratory arrest occurs in the absence of a recorded decision there should be an initial presumption in favour of attempting CPR.
- Anticipatory decisions about CPR are an important part of high-quality health care for people at risk of death or cardiorespiratory arrest.
- Decisions about CPR are sensitive and complex and should be undertaken by experienced members of the healthcare team with appropriate competence.
- Decision about CPR require sensitive and effective communication with patients and those close to patient.
- Decision about CPR must be documented fully and carefully.
- Decisions should be review with appropriate frequency and when circumstances change.
- Advice should be sought if there is uncertainty.
11.8 Appendix H Do not attempt cardiopulmonary resuscitation form (WZT652)
11.9 Appendix I Do not attempt cardiopulmonary resuscitation communication sticker
11.10 Appendix J What if my heart stops leaflet
This leaflet has been produced to help you understand what happens when your heart stops beating, how cardio-pulmonary resuscitation (CPR) can be used, and when it may not be helpful.
It may be upsetting to talk about resuscitation. This booklet tries to explain the issues as clearly and sensitively as possible.
You do not have to discuss resuscitation if you do not want to. However your health care team is available if you change your mind.
11.10.1 Why do people die?
It’s sad, but everybody dies.
Thinking about dying usually makes us sad, and perhaps a bit frightened.
It’s not something we like to think about, but talking with your family or with your doctor, and making plans for that time, can make things as easy as possible for you and those close to you.
Death might be due to an accident, or a sudden event, but most people die from serious illnesses which they have had for many months or even years.
11.10.2 What happens when my heart stops beating?
When you die your heart stops beating.
No blood gets pumped round your body, so very quickly the rest of your body stops working.
Your kidneys, your liver, your lungs all stop working.
Your brain will stop working about three minutes after your heart stops beating.
11.10.3 What is cardiopulmonary resuscitation (CPR)?
If your heart stops beating it may be possible to start it beating again.
Attempts to restart your heart will include pressing down firmly on your chest again and again, and breathing for you.
This is called cardiopulmonary resuscitation (CPR).
Ambulance or hospital staff might use a machine to give your heart an electric shock to make it start working again.
They may put a tube down your windpipe to help you breathe, or give you drugs to help your heart start.
11.10.4 Do patients fully recover after cardiopulmonary resuscitation?
Each person has a different chance of cardiopulmonary resuscitation (CPR) working. Only about 2 out of 10 patients who have CPR survive and go home from hospital; survival is less likely in people with lots of health problems.
Even if CPR starts the heart again, patients usually need more treatment, often in an intensive care unit. Some patients never get fully better and suffer from mental or physical disabilities.
The decision to attempt CPR has nothing to do with how old you are or your abilities. It is about whether the treatment will help you.
Your doctor is the best person to decide if CPR is likely to help.
CPR will not be attempted if it will only start your heart and breathing for a short time, or if it would prolong your suffering.
11.10.5 Will someone discuss cardiopulmonary resuscitation with me?
You might want to talk about what happens when you die, or you might have questions about CPR. It might be that because you have lots of health problems, CPR cannot help, and the health care team will decide not to attempt it when your heart stops. This is a do not attempt cardiopulmonary resuscitation (DNACPR) decision.
You have a right to be told if a DNACPR decision has been made, unless telling you would be harmful.
11.10.6 What if I don’t want to or am unable to talk about this myself?
You can appoint someone to have power of attorney for your health. This person is then allowed to speak on your behalf when you can’t do this yourself. If you cannot talk for yourself or don’t wish to, then the health care professionals in charge of your care will decide what treatment is best for you (this is a best interests decision). Wherever possible they will discuss this with those close to you.
11.10.7 What if I want cardiopulmonary resuscitation to be attempted?
Health care professionals will not refuse your wish for cardiopulmonary resuscitation (CPR) if it will be of benefit to you.
However, you cannot insist on having a treatment that will not work. Health care professionals will not offer treatment that will be degrading or cause harm.
If there is any doubt that CPR would work, the health care team can arrange a second opinion if you would like one.
If CPR might work, but it is likely to leave you severely ill or disabled, your opinion about whether the chances are worth taking is very important.
The health care team must and will listen to your.
11.10.8 What if I know I don’t want to be resuscitated?
If you don’t want CPR you can refuse it and your health care team must respect your wishes. You can talk to your doctor or nurse about this.
Your doctor or nurse can give you advice on making a legally binding advance decision to refuse treatment.
11.10.9 If it is decided cardiopulmonary resuscitation (CPR) will not be attempted, what will happen next?
If you do not want CPR, or if your doctor decides that it will not work for you, a do not attempt cardiopulmonary resuscitation (DNACPR) form will be completed and discussed with you.
It tells everyone who looks after you that this decision has been made.
There is only one copy of the form which will be needed if you are admitted to hospice or hospital, or if you travel by ambulance. At home, it needs to be kept safe so that healthcare professionals can see it if needed.
11.10.10 What happens if my situation changes?
Your DNACPR form will state when the decision should be reviewed. If your health condition changes, the decision can be reviewed.
Your health care team will be happy to discuss any changes with you.
11.10.11 Can I see what is written about me?
You have a legal right to see what is written about you and can ask to do so.
If you do not understand what is written, your health care team will explain it to you.
11.10.12 What about other treatments?
If doctors decide not to attempt CPR, this will not affect any of your other treatment.
You will still receive the best care and medicines for your condition.
11.10.13 Who else can I talk to about this?
If you or your family do not think that you have had a chance to talk about this properly, please talk to a nurse or doctor looking after you.
If you don’t want to talk about it at all, that’s fine too.
There are people to listen if and when you do:
- your family, friends and carers
- a hospital chaplain, or someone from your own faith community
- an advocacy service
- community nursing teams
- palliative care teams
- your GP
- your district nurse
This leaflet has been adapted from an original collaboration between The Bradford and Airedale Palliative Care Managed Clinical Network for People with Learning Disabilities and Bradford Taking Media’s Access to Information for Minorities (AIM) Project.
The Yorkshire and Humber DNACPR Regional Working Group gratefully acknowledges the work of these groups.
11.10.14 References and further reading
11.10.15 Document control
Decisions relating to cardiopulmonary resuscitation, RCN, Resuscitation Council (UK), BMA 3rd edition 2014 Deciding right, your life your choice. NHS England Northern Clinical Networks and Senate, April 2014.
11.11 Appendix K Where to document the do not attempt cardio-pulmonary resuscitation (DNACPR) decision in the electronic records
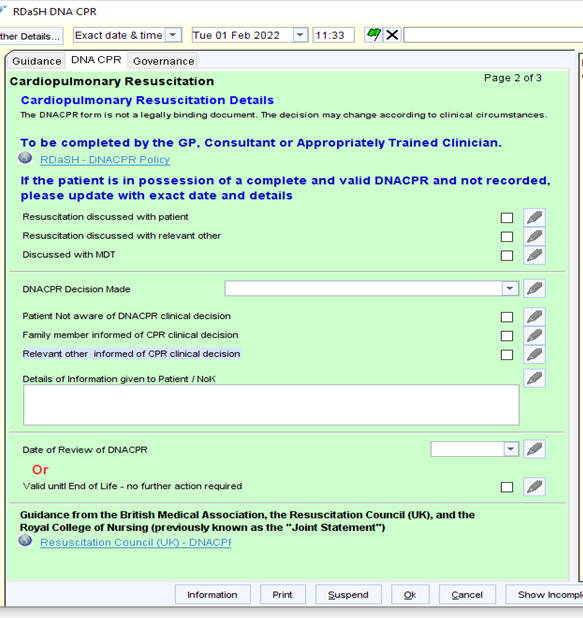
- Search for DNACPR in templates or locate RDaSH DNACPR in the left-hand clinical tree under corporate templates.

- Right click on RDaSH DNACPR.
- Click again on RDaSH DNACPR.
- The green information box will come up.

- Click the grey DNACPR tab at the top.
- This page gives a guide to DNACPR. The grey tab goes to the page to be completed, see next page.

- Tick the relevant boxes.
- Select the correct action from the drop-down menu, for example, not for attempted CPR.
- Write the details of the conversation with the patient or those closest to them, or the review on an existing document in the ‘detail of information’ box.
- If having a review date, tick the box.
- If valid until the end of life, tick the box.
- Press OK and Save as normal.
11.12 Appendix L Do not attempt cardiopulmonary resuscitation child under 16 letter
Document control
- Version: 1.1.
- Unique reference number: 1011.
- Approved by: Clinical policies review and approval group.
- Date approved: 20 February 2024.
- Name of originator or author: Medical director and Resuscitation Committee chair, consultant in palliative care and Resuscitation Committee deputy chair, resuscitation officer.
- Name of responsible committee or individual: Chief nurse.
- Date issued: 27 February 2024.
- Review date: June 2025.
- Target audience: All staff.
Page last reviewed: March 12, 2025
Next review due: March 12, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.