Contents
1 Introduction
A pressure ulcer is localised damage to the skin and, or underlying tissue, usually over a bony prominence (or related to a medical or other device) resulting from sustained pressure (including pressure associated with mechanical force of shear). The damage can present as intact skin or an open ulcer and maybe painful (EPUAP2019).
Pressure damage is common in many health settings, affecting all age groups, and is costly in both terms of human suffering and resources. Most pressure damage could be prevented and it is important to have prevention and educational strategies in place based upon the best available evidence.
2 Scope
This procedure is intended for use predominantly in the community, Tickhill Road Hospital site in-patient services and provides guidance for other patient areas covered by the trust. However, it may also be relevant for all other in-patient services and the need for a pressure ulcer risk assessment will be determined by the physical assessment on admission, in line with the policy minimal standards for the physical assessment, examination and ongoing care of in-patient in mental health and learning disability service.
In the North Lincolnshire and Rotherham localities tissue viability and wound care services are provided by North Lincolnshire and Goole NHS Foundation Trust and Rotherham NHS Foundation Trust. The tissue viability and wound care services provided are a combined hospital and community service.
3 Link to overarching policy, and or procedure
3.1 Wound care and tissue viability manual
3.2 Links to relevant policies or procedures
- First to dress initiative procedure (TVWC manual)
- Wound management procedure (previously wound management policy)
- Wound photography using smartphone or digital device procedure (TVWC manual)
4 Procedure or implementation
For the prevention and management of pressure ulcers. Following the structure of stop the pressure (ASSKING):
- A, assess the risk to pressure injury
- S, surface look at all the surface the person comes in contact with
- S, skin inspection for early detection
- K, keep moving or assist to change position Incontinence or moisture management
- I, incontinence or moisture management
- N, nutrition a heathy diet and hydration
- G, giving information at a level that enables the person to make informed choices and participate in care planning (Royal Marsden 2020)
Individual care plans will be developed from the nursing assessment, taking into account the patient needs, preferences and legal requirements. This personalised prevention plan may include a pressure-relieving device.
Pressure relief equipment is supplied in the community in partnership with the providers of community loan equipment for the prevention and management of pressure ulcers.
4.1 Assessment of pressure ulcer risk
The qualified nurse will perform an initial risk assessment in first episode of care, on admission to inpatient areas within 6 hours for planned admissions and at first visit for community patients. (This may be extended up to 12 hours if the patient’s mental health state will not allow it to be undertaken within 6 hours). If the clinical presentation of the patient is high risk for example immobile, unconscious or critically ill then prevention strategies must be implemented immediately.
Risk assessment is a fundamental part of preventing pressure ulcers and prescribing care. Many pressure ulcer risk assessment scales have been developed, but these represent only one part of the process. Individual’s risk of developing a pressure ulcer can change over a short or long period of time. It is linked with the general health and wellbeing of the individual in the majority of cases; however small changes in care or routine can dramatically increase risk. Once recognised these factors should be removed if possible or reduced as much as possible.
The trust supports the use of Pressure Ulcer Programme of Research Tool Purpose T V2 adapted from University of Leeds and Leeds Teaching Hospitals NHS Foundation Trust as the pressure ulcer risk assessment tool and is supported by the NWCSP (2022).
Completion of Purpose T will give a direction for care planning:
- green pathway, on assessment no pressure ulcer identified and not currently at risk
- amber pathway, on assessment no pressure ulcer but at risk and primary prevention pathway with care plan to minimise or eliminate risk within principles of skin, surface, keep moving, incontinence or moisture, nutrition
- red pathway, pressure ulcer category 1 or above or scarring from previous pressure ulcers with care plan for secondary prevention to minimise or eliminate further risk within principles of skin, surface, keep moving, incontinence or moisture, nutrition and a management care plan for treatment of pressure ulcer
Review risk assessment in line with care plan notification, for example, in line with complexity score in the community, with changes in clinical condition for example patient becomes unwell, develops incontinence or reduction in mobility or nutrition.
All patient’s prevention or treatment management. Patients with identified risk factors may require referring to other members of the health care team. Referrals to a dietician for all grade 3 and above pressure sores, physiotherapist, occupational therapist or continence advisor should be made where appropriate.
Risk status can increase or decrease; both may require changes in care.
4.1.1 Appendix B Pressure ulcer risk primary or secondary evaluation tool (Purpose T V2)
Patients wearing prescribed anti-embolic stockings for up to 23.5 hours a day, they require removal, for a maximum of 30 minutes in a 24-hour period to allow the legs and feet to be washed and skin condition and integrity observed.
Document all findings:
- staff should be aware of the following signs on the skin which may indicate early development of pressure ulcers.
- persistent erythema (redness)
- non-blanching hyperaemia previously identified as non-blanching erythema (redness)
- blisters
- discolouration
- localised heat
- localised oedema
- localised induration
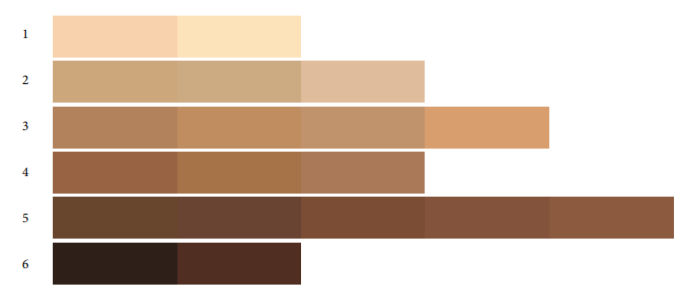
Assessment should involve a thorough inspection of the skin, and this should include finding out about the patients’ baseline skin tone following the skin tone tool (adapted from Ho and Robinson, 2015). Patients with darkly pigmented skin have a high melanin concentration in the skin, which makes it difficult to detect erythema, the main indicator of pressure damage. There are other signs and symptoms that can be observed:
- purplish or bluish localised areas of skin
- temperature change, initial warmth due to the inflammatory response which will become cooler as tissue death occurs
- localised oedema due to the inflammatory response
- localised induration due to excessive inflammation and necrosis (Wounds UK 2021)
Full assessment of skin areas can often involve removal of clothing, surgical appliances and mobility aids. Assessment should not only be visual as pressure ulcers can often be felt as soft and boggy. Persistent redness (erythema) does not always lead to ulceration but must be closely observed.
Other causes of skin damage and redness may be from incontinence rather than pressure incontinence associated dermatitis (IAD), any area of abnormal skin should be examined by a registered nurse and documented.
4.2 Surface
4.2.1 Pressure relieving devices
Support surfaces for beds and chairs must reflect the patient’s pressure ulcer risk and ability to change position. If a patient cannot reposition independently then consider the use of dynamic mattress systems where two hourly repositioning is not feasible.
Devices (mattresses and cushions) come in two main types; those that reduce pressure by spreading the weight and increasing the surface area, and those that relieve pressure by removing the pressure at frequent intervals. Decisions about which pressure redistributing device to use should be based on an overall assessment of the individual and not solely on the basis of scores from risk assessment scales.
Consider smoking status and suitability of equipment and refer to fire service for advice (a risk assessment is in development but not available as yet, in the meantime if support required contact TVALS or NRS).
Pressure relieving equipment does not replace the need for repositioning and should be used as in conjunction with repositioning and skin inspection regime that suits the patient and circumstances.
Pressure relief equipment is supplied in the community by the community loan equipment loans service. Details of equipment provided and ordering procedures are included in the online Nottingham Rehabilitation Society (NRS) IRIS electronic catalogue. If the patient lives outside the geographical area, contact NRS to ask for guidance on who to contact to order equipment.
Only authorised staff with an individual personal identification number (PIN) can order equipment via NRS. Staff must attend training before they are issued with a requisition number and will be expected to attend periodic refresher training to retain their Requisitioner status.
Within the Doncaster in-patient area pressure relieving equipment is available on the ward.
4.2.2 Equipment selection
Before equipment is chosen existing support surfaces (bed, chair) should be examined for suitability. Lack of support and bottoming out from an old mattress or cushion could be causing the pressure damage.
All vulnerable patients, including those with a category 1 to 2 pressure ulcer should receive, as a minimum provision, a high specification foam mattress and the ulcer should be closely observed for deterioration.
The level of equipment support should be increased (stepped up) when:
- the patient is showing signs of pressure damage
- as a first line preventative strategy for persons identified at elevated risk
- the patient’s condition deteriorates
The level of support should be decreased (stepping down) when:
- the patients condition improves
- mobility improves
- post operatively (over 24 hours)
- following successful rehabilitation
Adverse incident reports using the reporting system Ulysses system (IR1s) should be raised to report the:
- equipment failures
- non-compliance with manufacturer’s instructions
- misappropriate use of equipment, for example, allocated equipment is not with the named patient
- prescribed pressure relief equipment is not available in a timely manner
There are three principles of action when selecting a pressure relief device for pressure ulcer prevention and, or management:
- reducing or relieving pressure
- preventing damage to the skin
- improving tissue resistance
Decisions about support surfaces should be made following a holistic assessment of a person’s risk, comfort and general health state.
Patient movement in and out of bed should be considered as air mattresses can restrict movement.
Assessment should be ongoing throughout an individual’s episode of care and the type of pressure relief support changed to suit any alteration in risk.
Patient may choose not to use any therapy products because of their personal circumstances in particular those that wish to continue sleeping with their partner.
A full conversation about risk and consequences should be discussed with the patient. If you believe the patient has capacity to make decisions about their care and treatment of the pressure ulcer you should ask the and patient to sign informed refusal form, within the consent to care and treatment policy. The risks and consequences need to be revisited on a regular basis and the person capacity ability to consent reconsidered.
Where there are concerns about the person capacity a mental capacity assessment should be undertaken and recorded on the MCA1 questionnaire on SystmOne in line with the MCA Mental Capacity Act 2005 policy.
If the outcome is the person has capacity, then you proceed with informed refusal process, if they lack capacity then a best interests decisions to whether they should receive the treatment against their wishes should be carried out and recorded on MCA2 (Best interests decision record).
A bed rail risk assessment should be completed and appropriate bed rails supplied.
4.2.3 Electric profiling beds
Electric profiling beds reduce skin damage by:
- making movement easier for the patient, carers and staff to perform, reducing friction and shear
- use of the knee break prevents sliding down the bed reducing friction and shear
- allowing patients to change their own position
- it is vital that an environmental check be carried out to ensure space is available as these beds a larger than a standard divan and require additional space for functionality
- for patients with category 4 pressure injury the profiling bed base is supplied with a pressure relief mattress replacement system
- equipment and mattresses available in the in-patient areas should be cleaned in line with latest guidance from infection prevention and control
- equipment allocated from community loan equipment services should be returned at the end of allocation for cleaning and decontamination
- healthcare professionals are responsible to ensure that equipment prescribed for patient is documented on electronic record and checked this remains in working order
- healthcare professionals have a duty of care to their patients when using pressure reducing or relieving equipment to ensure it is used safely and appropriately. Information leaflets provided should be read and adhered to and all healthcare professionals should be able to trouble shoot routine and minor equipment failures
- most pressure reducing or relieving systems are fitted with visual and, or audible alarms and informal and formal carers should be informed of whom to contact should the alarms be activated
- prescribed equipment should be monitored for safe and effective working order at each community visit and reassessment of appropriate allocation in-line with at risk status or pressure ulcer management plan as a minimum in line with patients community complexity score review
- foam mattresses should be checked for collapse of foam (bottoming out use both fists to lean weight on mattress and test to feel base of bed frame) and integrity of cover on at least a monthly basis
- mattress with a ripped or torn cover through to the foam need to be condemned and replaced this is due to the risk of contamination to the foam
- pressure relief system covers that are ripped or torn also require replacement because of risk of contamination
- electrical equipment requires an adequate electrical supply and should be plugged directly into the electrical socket. Consider the safe positioning of trailing wires either around or under the bed. All wires should be secured and neatly placed
All manual handling tasks should consider the whole picture and assessed using the ergonomic framework of; task, load, individual, environment and equipment provision. Giving consideration to the environmental factors for example, space around the bed and mattress.
All equipment provided by NRS, cleaning instructions for all equipment is provided on delivery for patients family and clinicians to follow.
4.2.4 Seating pressure relief
- The benefits of a pressure redistributing device should not be undermined by prolonged chair sitting.
- When sat in a chair 70% of your body weight is spread over 8% of your surface area. This means that seating increases the risk of pressure damage. Poor seating increases the risk even more.
- When planning to sit a patient out of bed consider the following points:
- the severity and location of any pressure ulcers
- the patients’ ability to sit comfortably in an armchair and reposition themselves
- ergonomics of the chair, for example, height, depth, width, position of armrests
- ease of transfer from bed to chair and the use of appropriate moving equipment
- posture, mobility, comfort and support.
- functions required when sitting, for example, eating or washing
- patient choice and psychological consideration
- A patient considered at high risk who is provided with an alternating pressure mattress but who sits out should also have their seating assessed and suitable equipment provided.
- Patients should be advised of the risk of prolonged chair sitting so they can make informed choices about it.
- NICE recommend restricting the time spent seated to a maximum of 2 hours at a time for high-risk patients
- Advice should be sought from the multidisciplinary team (occupational therapists, physiotherapists, wheelchair services) if seating is a problem.
4.3 Skin
| Action | Rationale |
|---|---|
| Verbally check the identity of the patient by asking for name and date of birth. If not possible, check details with family or carers, community. Check patients ID bracelet, in-patient area | To confirm that the patient is correct recipient for procedure |
| Ensure patient is introduced to staff involved in procedure by name | Improves communication and helps reduce anxiety |
| Give clear explanation of the procedure to be performed to gain valid consent, including any risks and the care that will follow | To gain patient co-operation and enable informed and understood consent to the procedure |
| Record outcome of discussions and document in care plan, including consent to procedure | Record in health record for accurate information |
Treatment of the skin therefore depends on the state in which it is found, rather than routine procedure. The following principles in caring for the skin:
- keep it clean
- do not let it remain wet
- do not let it dry out
- prevent accidental damage
- skin inspection can take place during routine care taking into account patient consent, preferences, privacy and dignity
- refusal to allow skin inspection should be documented, and the risks fully explained to patient and carer(s)
Skin assessment for individual identified at risk should be carried out after each position change; this will allow the practitioner to guide decisions on the length of time between each position change. Completion of repositioning chart will assist in care planning for assessment of pressure areas identified as high risk.
In the community when working in partnership with other agencies, the compliance and documenting of turns and repositions and the effectiveness of the regime, to be reviewed and recorded at each visit.
Patient should have a turning or re-positioning regime and pain assessment related to the pressure ulcer or its treatment. Manage pain by eliminating or controlling the source and offer pain relief as appropriate. Seek specialist advice if necessary. Document all findings in electronic records.
Where a red area is noted, apply light finger pressure for 10 seconds if the area blanches, goes pale, on removal of finger there is no damage to micro, circulation. If the area remains red, non-blanching erythema of intact skin, a category 1 pressure ulcer is indicated and further action is required.
Correct positioning and support is important to minimise friction and shear whether in bed, chair and wheelchair. This includes the use of pillows to keep bony prominences apart (for example knees, heels or ankles). However, care should be taken to ensure that these do not interfere with the action of any other pressure relieving equipment in use. Patients at risk of developing pressure ulcers because of the time spent sitting in a chair should be encouraged to sit in a chair, which is of the correct height in addition to the use of a pressure relieving device.
4.4 Keep moving
Individuals, where appropriate should be encouraged to reposition themselves if this is possible.
Consideration should be given to the prescribing of TOTO™ (this is lateral turn equipment that is placed on the bed base between the bed frame and the mattress or pressure relief system) to provide assistance with a turning and repositioning regime.
The use of the 30-degree tilt has been found to be beneficial to the patient. It involves the patient being positioned at a 30-degree angle using pillows, rather than at a 90-degree angle which would place them directly onto their hip and therefore at increased risk. (Preston 1988).
4.5 Incontinence
Where incontinence and, or moisture to the skin is identified as a risk factor advice can be sought from the continence specialist services.
As per pathways within the Doncaster Wound Care Formulary September 2022, to be reviewed July 2024. Skin Care Pathway for Incontinence Associated Dermatitis (IAD) and Moisture Associated Skin Damage (MASD)
4.6 Nutrition
Malnutrition and dehydration are risk factors for the development of pressure ulcers. To help achieve healthy nutritional status for the patient:
- promote a healthy balanced diet
- encourage staying hydrated; aim to have 6 to 8 drinks (1.5 litres) per day, this could include water, tea, coffee, milk and, or juice
- if appetite is poor; encourage an enriched diet with high calorie snacks and drinks (high in fat and sugar), for example, milky drinks and dairy based puddings
- if overweight or obese advise to follow healthy eating guidance, for example, have the right portion size, choose low fat dairy foods, avoid high sugar foods, for example, biscuits, cakes, chocolate, fizzy drinks, sweets. However, if a person is identified to be at risk of malnutrition following screening (for example, 5 to 10% or more weight loss in the last 3 to 6 months), avoidance of these foods may not be appropriate in the first instance. Please refer to the must template and care plans available for guidance
- if a patient is unable to eat independently consider suggesting purchasing adapted cutlery or crockery to support independence, provide assistance prompting encouragement or feeding when needed
- if patient is in own home and unable to eat independently
- refer onto the relevant service if these are the primary reasons for low intake, for example, dentist, speech and language therapy, mental health team, GP
All patients on initial assessment should have nutritional assessment completed using must assessment tool. All patients who are nutritionally compromised should have a plan of appropriate nutritional support or supplementation that meets the individual needs and is consistent with overall goals of therapy. Referral to the dietetic service should be made as appropriate. Patient’s receiving late stage (last 12 weeks) palliative care should be provided with the nutrition in palliative care leaflet (must page 1).
4.7 Giving information
Education for staff within the trust.
Pressure ulcer awareness education tier 1,2 and 3 This will form part of the professional role requirements training, tier level to be decided by service manager.
These learning objectives are based on the recommendations from the national wound care strategy programme core capabilities Framework for England (2021).
This framework is used by the Doncaster Wound Care Alliance. The framework has been designed to cover all health and social care settings. It is up to the practitioner and their employer to determine which tier of knowledge and skills they need to achieve within their current role.
The capabilities are cumulative; therefore, a health or care practitioner working at tier 3 will be able to demonstrate the capabilities at tier 1 and tier 2 as well as those at tier 3. The Tiers do not relate to specific roles or pay grades.
| Tier 1 | Tier 2 | Tier 3 |
|---|---|---|
| Capabilities that require a general knowledge and understanding of wound care and the skills which support provision of care, the focus being on pressure ulcer risk.
We propose this could be achieved by awareness El earning including information on wound photography and supported by leaflets which may be provided to the patients or carers. This e-learning awareness video will include:
|
Capabilities that enable the provision of wound care independently and with a degree of critical analysis. Using the see treat and refer on model.
We propose this could be achieved by a more comprehensive E learning, which builds on the tier 1 content. Supported by the provision of the WRAP pack on completion of the e-learning. This e-learning will include
|
Capabilities that require a high degree of autonomy and complex decision-making, an ability to lead wound care practice, enabling innovative solutions to enhance people’s experience and improve outcomes.
This is a face-to-face taught session which focuses on the risk assessment, avoidance of risk and if a pressure ulcer develops the care, treatment, reassessment, reporting and duty of candour process. This is part of the wound care alliance training programme for district nurses. This will be rolled out to the physical health wards by learning and development in 2023. This formal teaching session includes:
|
| e-learning on ESR pressure ulcer awareness, caring for skin and preventing pressure ulcers | e-learning | Taught session |
| Learning objectives care of skin and prevention of pressure ulcers | Learning objectives Tier 1 plus | Learning objectives Tier 1 and 2 plus |
| Adhere to local protocols, policies, guidelines, and relevant regulatory frameworks relating to wound care and treatment. First to dress initiative procedure (TVWC manual) | Understand the anatomy and physiology of the skin, the importance of maintaining its integrity | Construct, oversee and advise upon the development of wound care management plans in collaboration with the multidisciplinary team, which include specific review dates |
| Understand common terms | Be able to recommend and carry out agreed wound management techniques and therapies within the scope of practice | Develop care plans that take account of the individual’s needs, goals and wishes, local service availability and relevant guidelines, ensuring that the management plan considers all options that are appropriate for the care pathway |
| Identify who is most at risk of developing a pressure ulcer | Make timely and appropriate wound management referrals | Have a comprehensive knowledge of the wound healing process and other factors which can affect healing |
| Know when to react to at risk skin | Have a comprehensive knowledge of local and regional wound care protocols and guidance (wound care formulary) | Engage in the critical review of own and others’ practice, learn from them and share the learning with colleagues and networks |
| Understand the ASSKING bundle and how to use it | Know where to refer onto for ongoing care and treatment | |
| Know where to get help |
||
| Posed target audience | Proposed target audience | Proposed target audience |
| Clinical staff who see patients or clients who would follow health promotion advice or who have carers or parents who can follow the advice and give the direct care. For example, health visitors, those who would not directly provide first line physical health care. | Clinical staff who see patient or clients who would be at risk of pressure ulcer damage but would be unable to follow health promotion advice and would require more clinical assistance. They would follow the first to dress policy, provide first line care, following the “see, treat, refer on” pathway. They would be provided with the core WRAP pack for first line dressings. They would not provide ongoing wound care and advice, for example, specialist nurses, AHPs | Clinical staff who wound care and wound dressings are part of their core role. They would provide ongoing wound care and advice to patients cares and families. They would follow the Doncaster wound care formulary and have access to a dressing store, equipment provision. For example, district nurses, physical health in patient areas, hospice staff, TVALS |
Individuals who are willing and able should be encouraged, following education and guidance, to inspect their own skin and pressure points. Where practicable the patient and their family or carers should be involved in the inspection process. Any education or guidance should be recorded and supported with written information. This should include the importance of reporting to the healthcare professional any areas of concern.
Patient or carers or family can be directed to under pressure video (opens in new window) for visual information on the formation of a pressure ulcer and their prevention and detection.
Patient or carer or family information to compliment the video is available in leaflet format react to RED.
4.7.1 Appendix C React to RED leaflet for patient and carers
For patients presenting with poor nutrition the trust produce a leaflet with suggested food items to support an enriched diet.
4.7.2 Appendix D Food first
For patients who may present with challenges because of dementia the trust produce a leaflet with suggested food types and techniques to assist the patient achieve a nutritionally balanced diet.
4.7.3 Appendix E Eating, drinking and swallowing awareness in dementia
It is important to give relevant information in a way that patient can understand to make significant decisions about their health and welfare. Staff will record in the appropriate document or care plan the patients and carers understanding and comprehension of pressure ulcer prevention and, or management plans.
This to include information on the patient’s capacity to understand the information to ensure informed choice. The patient’s capacity to be recorded on completion of mental capacity form if appropriate (MCA form on electronic record).
Staff will record in the appropriate document or care plan efforts to re-enforce the principles and activities needed for an effective management care plan.
When a patient or principle carers decline to take on board the recommendations relating to pressure ulcer prevention or management, for example, use of pressure relief equipment, limit the time spent sitting in a chair.
After explanation of the advice provided, the potential benefits and the probable risks of not following the recommendations they should be given the opportunity to record their preferences by completing the informed refusal form available on TPP SystmOne.
The issues covered by the informed refusal form need to be revisited at least monthly, to ensure the accurate records of patient’s preferences and choices.
4.8 Guidelines for specialist patient groups
4.8.1 Critically ill patients
Consider the need to change support surfaces for patients who cannot be turned for medical reasons such as spinal instability, for example, spinal cord compression and haemodynamic instability.
Consider more frequent small shifts in position to allow some re-perfusion in patients who cannot tolerate frequent major shifts in body positions, for example, utilise 30-degree tilt techniques.
Prevent shear injury with the use of slide sheets for any repositioning move.
If patient presents with a pressure ulcer or wound, document the number of dressings and their position if filling undermining areas to ensure they are correctly removed at next dressing change. Do not pack tightly as this will cause additional pressure.
4.8.2 Bariatric obese patients
Ensure adequate assistance to fully inspect all skin folds. Pressure ulcers may occur in unique locations, such as beneath folds of skin and in locations where tubes and other devices have been compressed between skin folds.
Pressure ulcer develops over bony prominences, but may also result from tissue pressure across buttocks and other areas of high adipose tissue concentration.
Consider the use of pillows or other positions devices to off load large skin folds and prevent skin on skin pressure, for example, Kerrapro.
Ensure the correct fit of the bed that supports the weight of the individual and ensures sufficient width to allow turning and patient does not rest up against side rails of the bed when turned from side to side.
4.8.3 Patient receiving palliative care
Complete a comprehensive assessment of patient’s health status and combine this with patient’s preferences in turning, including whether they have a position of comfort after explaining the rationale for turning.
Establish a flexible repositioning schedule based on the patient’s preference and tolerance and the pressure redistributing characteristics of the support system. Individualise the turning and repositioning schedule, ensuring it is consistent with the patient’s goals, wishes, administration of prescribed analgesia, current clinical status and combined co-morbidity conditions as medically feasible. Document turning and repositioning as well as the factors influencing these decisions, for example, patient wishes, medical need.
Comfort is of primary importance and may supersede prevention and wound care for patients who have been diagnosed as being the final stages of dying or who have conditions causing them to have a single position of comfort. If appropriate offer prescribed medication to the patient 20 to 30 minutes prior to a scheduled position change for patients who experience significant pain on movement.
Consider the following factors in repositioning:
- protect the sacrum, elbows, and greater trochanters, which are particularly vulnerable to pressure
- use positioning devices such as pillows as necessary to prevent direct contact on bony prominences and to avoid having the patient lie directly on a pressure ulcer (unless this is the position of least discomfort and the patients’ preference)
- use heel protectors and, or suspend the length of the leg over a pillow(s) to float the heel away from the bed surface
- use a chair cushion that redistributes pressure on the bony prominences and increases comfort for patients who are seated
- ensure the family and carers understand the goal(s) for the patient’s plan of care
For pressure ulcer care, pain management, odour control and exudate management are the main aspects closely related to supporting the patient’s comfort. Select extended wear dressings to reduce pain associated with frequent dressing changes. If consistent with the treatment plan provide opioids and, or non-steroidal anti-inflammatory medications 30 minutes prior to dressing changes or procedures and afterwards as prescribed.
Skin changes at end of life, located predominantly on coccyx or sacrum usually shaped like a pear, butterfly or horseshoe. They are a variety of colours including red, yellow, or black, are sudden in onset, typically deteriorate rapidly and usually indicate the death is imminent.
4.8.4 Spinal cord injured patients
Specialist wheelchair assessment services should individualise the prescription of a wheelchair and seating support surface and associated equipment for posture, pressure re-distribution and consideration for transfers for lifestyle needs.
Use of a wheelchair is imperative for spinal cord injured individuals, but sitting will need to be restricted when pressure ulcers are present on sitting surfaces. Ideally ischial pressure ulcers heal in an environment where the ulcers are free of pressure and mechanical stress.
Total bed rest may be prescribed to create a pressure free wound environment. However, this approach comes with potential physical complications, for example, muscle wasting, deconditioning, respiratory complications, psychological harm, social isolation and financial challenges if a period off employment is required.
Deconditioning is a complex process of physiological changes following a period of inactivity, bed rest or sedentary lifestyle. It results in functional losses in such areas as mental status, degree of continence and ability to accomplish activities of daily living. It is frequently associated with hospitalisation in the elderly. The most predictable effects of deconditioning are seen in the musculoskeletal system and include diminished muscle mass, decreases of muscle strength by two to five per cent per day, muscle shortening, changes in periarticular and cartilaginous joint structure and marked loss of leg strength that seriously limit mobility.
This creates a challenging dilemma for the patient and clinician to provide a balance between the physical, social and psychological need against the need for total pressure off loading. Consider referring to the surgeon for an opinion regarding surgical intervention.
Further information from the spinal injury association website (opens in new window).
4.8.5 Patients with dementia
Older people in general are at higher risk of pressure ulcers, particularly if they have difficulty moving. Dementia increases this risk further, especially as it progresses. Pressure ulcers are linked to dementia because of various associated problems:
- mobility as people with dementia may have difficulty changing position without help. This can include problems with walking, transferring between bed and chair, or repositioning themselves. Their movement may also be restricted by others for fear of falls
- frailty as a result of loss of protective fat and muscle loss and thinning skin
- poor diet and dehydration which reduce the strength and healing capacity of the skin
- incontinent because of the damage to the skin that can be caused by moisture
- poor blood supply with conditions such as diabetes
- agitation or restlessness with the behavioural rubbing often over heels and elbows
- medications that may cause sedation or drying of skin
- communication as the person may be less able to tell someone they are in pain When assisting a person with dementia to wash or dress take the opportunity to assess the skin at pressure points
Further information on the Alzheimer’s website (opens in new window).
5 Categorisation of pressure ulcers
5.1 Assessing the ulcer
All patients who present with a pressure ulcer should receive an initial and ongoing pressure ulcer assessment.
Pressure ulcers should be graded using the classification system in the European Pressure Ulcer Advisory Panel, National Pressure Ulcer Advisory Panel, Pan Pacific Pressure Injury Alliance (2014) classification system of pressure ulcer categories.
Establish the root cause of the pressure ulcer: if noted on transfer onto community caseload, or reason for first community visit or on admission to the in-patient area defined as inherited pressure ulcer; if developed whilst on active community caseload or an in-patient on the ward defined as trust acquired.
- Category 1, non-blanchable erythema of intact skin. Discolouration of the skin warmth, oedema, induration or hardness may also be used as indicators, particularly on individuals with darker skin.
- Category 2, partial thickness skin loss involving epidermis or dermis, or both. The ulcer is superficial and presents clinically as an abrasion or blister.
- Category 3, full thickness skin loss involving damage to or necrosis of subcutaneous tissue that may extend down to, but not through, underlying fascia.
- Category 4, full thickness tissue loss with exposed bone tendon or muscle extensive destruction. Often includes undermining and tunnelling. The depth varies by anatomical location.
Deep tissue injury (DTI): Intact skin with localised area of persistent non-blanchable deep red, maroon, purple discolouration or epidermal separation revealing a dark wound bed or blood-filled blister. Pain and temperature change often precede skin colour changes. Discolouration may appear differently in darkly pigmented skin. This injury results from intense and, or prolonged pressure and shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury or may resolve without tissue loss.
Unstageable pressure injury: Full thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough and eschar are removed a category 3 or category 4 will be revealed.
Unstageable and deep tissue injury (DTI) should be reviewed by a clinician with appropriate skills on a weekly basis to help identify a definitive pressure ulcer category (needs to be graded within 10 days).
Moisture lesions: Presents as intact skin with a history of incontinence or perspiration. Area blanches on finger pressure test. Moisture associated skin damage (MASD) should be counted and reported in addition to pressure ulcers. Where skin damage is caused by a combination of MASD and pressure, it is reported on the category of pressure damage.
| Likely to indicate pressure ulcer | Likely to indicate moisture lesion | |
|---|---|---|
| Causes, if pressure or shear and moisture are simultaneously present, the ulcer could be a combined lesion | Pressure and, or shear present | Moisture present. Urine, poo, sweat and, or exudate |
| Location, a combination of friction and moisture can result in moisture lesions in skin folds | Tends to be located over a bony prominence | Limited to the anal cleft and has a linear shape. Not located on a bony prominence Per-anal erythema and skin irritation caused by faecal matter |
| Shape | Limited to one area. Circular or regular shape, except friction damage | Diffuse, different superficial areas In a “kissing” ulcer shape, (copy lesion or butterfly or reflection) |
| Depth | Partial skin loss of top layer of skin, category 2 full thickness skin loss category 3 or 4 | Superficial particle thickness loss, which can deepen if infected |
| Necrosis | Occurs with pressure ulcers | No necrosis in moisture lesions |
| Edges, if friction is exerted on a moisture lesion, it will result in superficial skin loss | Edges tend to be distinct | Often irregular lesions, diffused or irregular edges |
| Colour | Red skin, non blanching category 1 | Erythema |
Medical device related pressure ulcer: a pressure ulcer that results from use of devices designed and applied for diagnostic or therapeutic purposes.
When sacral ulcer(s) do not show signs of healing when appropriate wound dressing and appropriate pressure relief is achieved, give consideration to other causative factors:
- medication, for example, nicorandal
- incontinence dermatitis, defined as an irritant dermatitis
- underlying medical condition, for example, renal failure
- consequence of medical condition, for example, cancer
For pressure ulcer presenting on lower limbs a Doppler or Medi ABPI or Vascular Assist and complete lower limb assessment blood supply before considering use of debriding wound care products as directed for treatment aims for limb necrosis in “Wound Management Guideline with TIMES”.
This is all recorded within the Skin IPOC.
TIMES is a wound assessment guide:
- T, tissue
- I, inflammation or infection
- M, management of exudate
- E, edge of wound
- S, surrounding skin
Appendix I Wound management guideline TIMES.
6 Documentation of pressure ulcer
Document the origin, length, width, depth, wound bed presentation and category (using the above classification system) in the patients care plan.
Follow minimum data guidance (appendices to be added) complete the skin IPOC (wound care integrated pathway of care IPOC) and record variances as they present.
Healing pressure ulcers should not be reverse graded. A category 4 pressure ulcer does not become a category 3 as it heals it should be described as a healing category 4 pressure ulcer. Reasons for deterioration in a pressure ulcer should be noted and if not expected a thorough reassessment should be undertaken.
All pressure ulcers within the trust category 2 or above must be reported using the trust’s safeguard electronic incident reporting system (IR1) recognising the occurrence of pressure ulcers as adverse events. The details of the incident registration number to be recorded as a reminder in the patient’s electronic records on Patient Home page.
Trust acquired category 3 and category 4 to be investigated by systematic judgement review with root cause analysis (RCA). The author of the report will present findings to the trust pressure ulcer systematic review panel to establish if there was a no lapse in care but lessons learnt or lapse in care which is followed up with injury being logged as serious incident within full investigation to timeline. Duty of candour process needs to commence.
The simple fact that a person at risk has a pressure ulcer, even a category 3 or category 4, or multiple pressure ulcers, more than 3 or 4 at a lower category or mixed categories, is not in itself a reason to suspect abuse or neglect. There are a number of factors to help decide whether it potentially indicates neglect or whether it indicates a need for care providers to improve practice.
These factors include:
- the person’s physical health and existing medical conditions
- any skin conditions the person may have
- any other signs of neglect, such as poor personal hygiene
- the appropriateness of their care plan and whether it has been properly carried out
- the person’s own view, and the views of their family and friends, on the treatment and care
Consider these factors against The Care Act, Three Point Check (for section 42 enquiry)
The safeguard duty applies to any adult who:
- has need for care and support (whether the authority is meeting any of those needs)
- is experiencing, or is at risk of, abuse or neglect
- as a result of that need is unable to protect themselves from either the risk of or the experience of abuse or neglect
Staff will record in the appropriate document or care plan the patients and carers understanding and comprehension of pressure ulcer prevention or management plans. This to include information on the patient’s capacity to understand the information to ensure informed choose. The patient’s capacity to be recorded on completion of mental capacity form (MCA form).
Staff will record in the appropriate document or care plan the distribution of patient or carer information.
Staff will record in the appropriate document or care plan efforts to re-enforce the principles and activities needed for an effective management plan.
When a patient or principal carers decline to take on board the recommendations relating to pressure ulcer prevention or management, for example, use of pressure relief equipment, limit the time spent sitting in a chair. After explanation of the advice provided, the potential benefits and the probable risks of not following the recommendations they should be given the opportunity to record their preferences by completing the Informed Refusal Form available on TPP SystmOne.
The issues covered by the Informed Refusal form need to be revisited at least monthly, to ensure the accurate records of patient’s preferences and choices.
7 Treatment of pressure ulcer
A patient with a pressure ulcer will also require preventative care plan as well as a wound treatment plan for pressure ulcer management. Patients with pressure ulcers should receive an initial and ongoing holistic assessment. This section of the policy should be used in conjunction with wound management guidelines.
Referral to tissue viability and lymphoedema service (TVALS) should be made when:
- patient has a category 3 or category 4 pressure ulcer
- patient presents with a deteriorating pressure ulcer
- patient presents with a difficult to manage pressure ulcer
- patient presents with concerns regarding neglect or safeguarding contributing issues to pressure ulcer development
- if patient refuses treatment seek advice from TVALS
7.1 Liaison between care settings
Pressure ulcer prevention and management is complex, frequently crosses care and professional boundaries and benefits from a multidisciplinary and collaborative approach to care.
Sharing information and documentation will ensure continuity between care settings and ensure an appropriate package is instigated.
When possible, communication should take place prior to transfer and, or discharge ideally the information should include:
- patient’s level of risk
- any equipment used
- skin condition
- plan of care, for example, moving and handling plan, member of MDT involved
- relevant social and cultural information including communication needs
- wound dressing regimes
- wound dressing supplies for one change, to allow time for further supplies to be arranged
8 References
- All Wales Tissue Viability Nurse Forum 2009 Guidelines for Best Practice: the Nursing Care of Patients Wearing Anti-Embolic Stockings.
- Bianchi J Cameron J (2008) Management of skin conditions in older population Wound Care Sept S6 to S14.
- Briggs S L 2011 When is a grade 4 pressure ulcer not grade 4 British Journal of Nursing Volume 20 No 20 S4 to S9.
- European Pressure Ulcer Advisory Panel (2019) Prevention and treatment with pressure ulcers: Clinical practice guideline.
- Hagisawa S, Fergus Pell M (2008), Evidence supporting the use of two hourly turning for pressure ulcer prevention Journal of Tissue Viability 17 76 to 81.
- Ho BK, Robinson JK (2015) Color bar tool for skin type self-identification: a cross-sectional study. J Am Acad Dermatol 73(2): 312 to 3.
- NHS Institute for Innovation and Improvement 2009 High Impact Actions for Nursing and Midwifery.
- National Wound Care Strategy Programme (2022) Stop the Pressure, Pressure Ulcers (opens in new window)
- NPSA (2009) Pressure ulcers under plaster casts SIGNAL.
- National Institute for Clinical Excellence 2003 Pressure ulcer prevention. Clinical Guideline 7 NICE London.
- National Institute for Clinical Excellence 2015 The prevention and treatment of pressure ulcers. Clinical Guideline 29 NICE London.
- MHRA Device Bulletin DB 2006 (06) (reviewed 2012) Safe Use of Bed Rails.
- MDA (1991) Device Bulletin 9801 Medical Device and Equipment Management for Hospital and Community based organisation London MDA.
- Preston KW 1988 Positioning for comfort and pressure relief: the 30-degree alternative.
- Royal Marsden 2020 Stop the Pressure.
- The Care Act 2014 RDaSH Intranet.
- Tissue Viability Society 2009 Seating and Pressure Ulcers: Clinical Practice Guideline.
- Sibbald RG et al. (2009) Skin changes at end of life SCALE Final Consensus Statement.
- Wounds UK (2021) Best Practice Statement Addressing skin tone bias in wound care: assessing signs and symptoms in people with dark skin tones.
- Wounds UK (2017) Quick guides: TIMES model of wound bed preparation.
- Young T (2017) Back to basics: understanding moisture, associated skin damage.
- Wounds UK Vol13: No 2: 56 to 65.
9 Appendices
Please see wound care and tissue viability manual webpage for appendices attached to this procedure.
- Appendix A Skincare protocol for incontinence associated dermatitis (IAD) primary care
- Appendix B Purpose T
- Appendix C REACT to RED patient and carer leaflet
- Appendix D Food first
- Appendix E Eating, drinking and swallowing awareness in dementia
- Appendix F Prevention of medical device-related pressure ulcers (MDRPU)
- Appendix I Wound management guideline TIMES
Document control
- Version: 2.
- Unique reference number: 508.
- Approved by: Clinical policy review and approval group.
- Date approved: 7 March 2023.
- Name of originator or author: Clinical nurse specialist (CNS) in tissue viability.
- Name of responsible individual: Clinical policy review and approval group.
- Date Issued: 26 March 2023.
- Review date: 31 March 2026.
- Target audience: All clinical staff.
Page last reviewed: January 09, 2025
Next review due: January 09, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.
Report a problem