Contents
1 Aim
In 2021, the Royal College of Paediatrics and Child Health (RCPCH) reviewed their guidance on perplexing presentations (PP) or fabricated or induced illness (FII) in children. The updated guidance provides procedures for safeguarding children who present with PP and FII and offers practical advice on when and how to recognise it, how to assess risk and how to manage these types of presentations in order to obtain better outcomes for children.
The aim of this procedure is to assist colleagues in fulfilling their statutory duties to safeguard and protect children and young people where there is a concern about PP or FII in children.
For the purpose of this procedure the legal definition of “child”, applies to those under 18 years of age. The term “children” applies to children and young people throughout this procedure and is anyone who has not yet reached their eighteenth birthday. If concerns around PP or FII are raised regarding an adult at risk then multi agency adult safeguarding procedures must be followed.
This procedure provides a framework for earlier intervention to explore the concerns of children, families, and professionals to address the issue of a PP before significant harm has come to the child or young person whilst also outlining when immediate action may be required.
This procedure is supplementary to national and local guidance and should be followed in conjunction with perplexing presentations (PP) or fabricated or induced illness (FII) in children guidance (RCPCH, 2021) (opens in new window).
2 Scope
This procedure applies to colleagues that are directly employed by Rotherham Doncaster and South Humber NHS Foundation Trust (RDaSH) and for whom RDaSH has legal responsibility. This procedure is also applicable whilst undertaking duties on behalf of RDaSH or working on RDaSH premises and forms part of their arrangements with NHS commissioners within Doncaster, Rotherham, and North Lincolnshire.
As part of good employment practice, agency workers are also required to abide by RDaSH policies and procedures, as appropriate, to ensure their health, safety, and welfare of those they care for, whilst undertaking work for RDaSH.
3 Link to overarching policy
4 Procedure
4.1 Spectrum of harm including perplexing presentations or medically unexplained symptoms and fabricated or induced illness
Some children may be presented for a medical review or intervention by their parent or carers when they are well. This can be due to over-anxious parents or carers, or a lack of understanding. Support may be required in order that the parents or carers are able to interpret and respond appropriately to childhood illness.
There will be occasions where a child or young person may present for medical attention, appointments, or surgical interventions with unusual or puzzling symptoms (medically unexplained symptoms or perplexing presentations). These are not attributable to any organic disease, and do not involve deliberate fabrication or deception but may also be indicators of FI, for example inappropriate use medication.
A key professional task is to distinguish between the over-anxious parent or carer who may be responding in an understandable way to a sick child and those parent or carers who exhibit abnormal behaviour that worry health professionals, for example, use of medical terminology not in keeping with language predominately used. Where it is identified that there are concerns about a parent or carer behaviour relating to the health of their child, agencies must work together in the best interest of the children. The perplexing situation or pathway must have oversight of a responsible clinician which will be either a paediatrician or children and adolescent mental health service (CAMHS) consultant dependent on if concerns relate to physical or mental health. In cases where the state and function of both physical and mental health is being explored then the most appropriate medic can be decided at a professionals meeting.
4.2 Medically unexplained symptoms
In medically unexplained symptoms (MUS), a child’s symptoms, of which the child complains, and which are presumed to be genuinely experienced, are not fully explained by any known pathology. MUS can:
- be physical or psych-social in nature
- include a huge range of symptoms
- may also include perplexing presentations (PP) or fabricated or induced illness (FII)
- affects 1 in 10 children
- like fabricated or induced illness, many fall victim to over-investigation
Health professionals and parents should work collaboratively to achieve evidence-based therapeutic work in the best interests of the child or young person. In 2018, the Royal College of Psychiatrists and the Paediatric Mental Health Association (PMHA) developed a guide to assessing and managing medically unexplained symptoms (MUS) in children and young people.
4.3 Perplexing presentation
The term perplexing presentations (PP) describes the commonly encountered situation when there are alerting signs (alerting signs are the presence of discrepancies between reports, presentations of the child and independent observations of the child, implausible descriptions and unexplained findings or parental behaviour) of possible fabricated or induced illness (FII) but the actual state of the child’s physical or mental health or neuro-development is not yet clear (but there is no perceived risk of immediate serious harm to the child’s physical health or life at this point).
Children and young people with perplexing presentations often have a degree of underlying illness, and exaggeration of symptoms is difficult to prove and can be hard for health professionals to manage and treat appropriately. In the absence of clear evidence about risk of immediate serious harm to the child’s health or life, the early recognition of possible FII (not amounting to likely or actual significant harm) is termed perplexing presentations.
Professionals may notice “alerting signs” of a perplexing presentation where:
- a child is being presented by a caregiver with symptoms and in some cases signs, that are inexplicable after all appropriate clinical examination and investigations have been carried out and no clinical cause having been found
- the symptom and symptoms complained of only occur in the presence of the caregiver. Despite arrangements for recording for example, seizures, there is usually no objective evidence for the clinician to assess
- the caregiver may also ask for and demand multiple health care referrals
- the symptoms reported are not borne out by the activities of the child as evidenced by others who are not the caregiver
- once a diagnosis has been proven not to be relevant, the caregiver persists in presenting it as an ongoing diagnosis when consulting with new professionals
- there is an exaggeration of symptoms and difficulties
- there may be a history of:
- change of address
- change of doctor and hospitals
- many out of hours attendances
4.4 Fabricated or induced illness
Fabricated or induced illness in children is a clinical situation whereby a child is, or is very likely to be, significantly harmed due to parental behaviour and action, carried out in order to convince doctors that the child’s state of physical and, or mental health or neurodevelopment is impaired or more impaired than is actually the case. This can involve:
- fabrication of signs and symptoms, this may also include fabrication of past medical history
- falsification of hospital charts, letters, documents and records including falsification of specimens of bodily fluids
- induction of illness by a variety of means, this includes poisoning and, or giving inappropriate medication
- often symptoms are seen in within the home and not observed by professionals in a clinical setting
- accounts of symptoms or illness given by the parent or carer and evidence such as photos cannot be confirmed as being the child in question
- a lack of the usual corroboration of findings with signs and symptoms or, a lack of usual response to proven effective treatments. It is this puzzling discrepancy that normally alerts the clinician to possible harm
- it can also include inadvertent harm caused by medical professionals such as unnecessary invasive investigations and, or procedures
FII involving deliberate deception of clinical services by the parent or carer to the child is rare but is a serious safeguarding concern and requires immediate attention and action.
4.5 Actions when fabrication of induced illness is identified
Where a practitioner suspects or observes that a child is at immediate risk of or has suffered significant harm particularly by illness induction for example, observed that medication tampered with given or without need, then the Police should be informed using the 999 service and a referral made to children’s social care as per local policy.
The RDaSH children’s safeguarding team should be informed via email: rdash.doncastersafeguardingchildren@nhs.net and a IR1 completed as per trust safeguarding procedures.
This is most likely to occur when there is evidence of frank deception, interfering with specimens, unexplained results of investigations suggesting contamination or poisoning or actual illness induction, or concerns that an open discussion with the parent might lead them to harm the child. The safety of siblings also needs to be considered.
All practitioners should be mindful of situations where informing the parents of the referral would place a child at increased risk of harm. In this situation, carers would not be informed of the referral before a multiagency discussion has taken place. This would usually be in the form of a formal strategy discussion.
4.6 Actions when perplexing presentation is identified
The RDaSH practitioner has made steps to engage with parent, carer or child to determine and provide any early help intervention or support required but perplexing presentations (PP) concerns remain around the health state and functioning of the child or children.
Where a practitioner has reason to suspect PP and further information or exploration is required, then they should first seek support and further advice from the RDaSH Safeguarding team via email: rdash.doncastersafeguardingchildren@nhs.net. The RDaSH Safeguarding team will discuss the concerns with the practitioner and advise of the appropriate actions to manage the perplexing situation.
If the PP pathway is to be initiated the practitioner will inform their manager.
4.7 If perplexing presentation is identified by children and adolescent mental health services (CAMHS)
The perplexing presentations (PP) pathway will be led by a children and adolescent mental health service (CAMHS) consultant, and they will be the responsible consultant (RC) at this stage.
The responsibility should not be delegated to a more junior member of staff although they may be involved in the process of assessment and subsequent management under the RC supervision.
The RDaSH children’s Safeguarding team should be informed via email: rdash.doncastersafeguardingchildren@nhs.net. The RDaSH Safeguarding team will discuss the concerns with the practitioner and advise of the appropriate actions for the PP pathway.
The Safeguarding team will have oversight of all PP and FII cases and will provide support and guidance throughout the process.
The responsible consultant must consider whether the parents or carers should be informed of any concerns regarding PP. Unless there is a risk of immediate, serious harm to the child’s health or life, parents or carers should be informed.
With support from the Safeguarding team, the RC must determine all relevant medical services involved with the care of the child (and siblings if appropriate) for example, general practitioners (GP), other consultants, and private doctors.
With support from the Safeguarding team, the RC must request relevant health information by sending a letter with an initial health information template to all involved health professionals, requesting a return within 10 working days of receiving the request (or sooner if necessary) (see appendix B and C).
The RDaSH initial health information template will be completed by the CAMHS Practitioner who identified the PP concerns with support from the RDaSH Safeguarding team.
RDaSH safeguarding team will collate all the returned templates.
The RC must arrange a multi-professionals meeting within 28 days (or earlier if the specific case demands an immediate assessment) of initial identification of concerns. All health professionals involved in the child’s care and the designated professionals from the integrated care board for safeguarding children should be invited.
The RC will lead the meeting. Clear terms of reference and records of the meeting must be made at the time and the arrangement for these will be made by the RC.
It should be decided in the meeting who Is the most appropriate person to be the RC depending on the nature of the PP, for example, mental or physical health presentations.
There may need to be one or more professionals’ meetings to gather information, reach a consensus and develop a rehabilitation plan. Where possible, families should be informed about these meetings and the outcome of discussions if doing so would not place the child at additional risk. Notes from meetings may be made available to parents, on a case-by-case basis and are likely to be released to them should there be a subject access request under the Data Protection Act (2018) for the health records.
The outcome of the meetings will reach a consensus about the child’s state of health. If the meeting concludes that there is reasonable cause to suspect that a child is suffering or likely to suffer significant harm, the RC must ensure that a referral is made to the local authority’s children’s services. Discussions with a senior colleague in children’s services may also be helpful in deciding whether, and when a referral should be made. The police public protection unit must be informed of any referral where fabricated or induced illness (FII) is suspected as this may also involve the committing of a crime.
If the meeting concludes that there is no reasonable cause to suspect that a child is suffering or likely to suffer significant harm, but the family require ongoing support, this should be considered within the professionals meeting and an ongoing health and education rehabilitation plan formulated.
All discussions and actions from the PP pathway should be recorded in the child’s health record on the safeguarding template so that other clinicians will have access to the information. Parent or carer’s access to the record will need to be restricted, and an alert should be added to reflect this. The terminology should focus on the category of abuse or medical neglect rather than PP and FII.
4.8 If perplexing presentation is by any other trust service
If concerns are around the child’s physical health then the PP pathway will be led by the child’s paediatrician or if not under the care of a paediatrician, a request will be made to the GP for a referral to a paediatrician with an overview of the concerns identified (see appendix D).
If concerns are around the child’s mental health then the perplexing presentations (PP) pathway will be led by the child’s children and adolescent mental health services (CAMHS) consultant or if not under the care of a CAMHS, a discussion with a CAMHS consultant will be requested to plan ongoing actions.
The RDaSH children’s safeguarding team should be informed via email: rdash.doncastersafeguardingchildren@nhs.net.
The safeguarding team will have oversight of all PP and fabricated or induced illness (FII) cases and will provide support and guidance throughout the process.
The RDaSH initial health information template will be completed by the practitioner who identified the PP concerns with support from the RDaSH Safeguarding team.
The RDaSH initial health information should be returned to the child’s paediatrician who will be the RC.
The RDaSH safeguarding team will support the medical professional at attendance at the multi-professionals meeting where the state of the child’s health will be discussed, and a consensus reached around actions for the family.
It should be decided in the meeting who Is the most appropriate person to be the RC depending on the nature of the PP, for example, mental or physical presentations.
All discussions and actions during the PP pathway should be recorded in the child’s health record on the safeguarding template so that other clinicians will have access to the information. Parent or carer’s access to the record will need to be restricted, and an alert should be added to reflect this. The terminology should focus on the category of abuse or medical neglect rather than PP and FII.
A flowchart of the process can be found in appendix A.
5 Appendices
5.1 Appendix A Flowcharts
5.1.1 Perplexing presentation concerns identified within children and adolescent mental health service
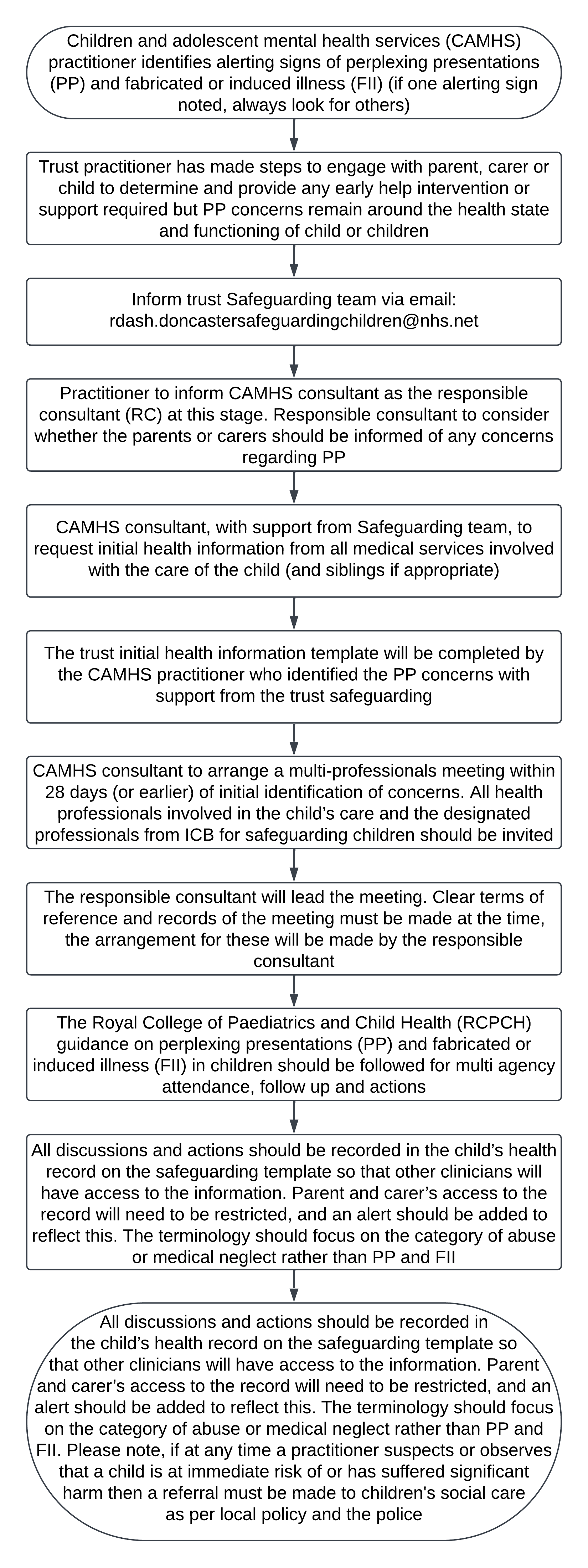
- Children and adolescent mental health services (CAMHS) practitioner identifies alerting signs of perplexing presentations (PP) and fabricated or induced illness (FII) (if one alerting sign noted, always look for others).
- Trust practitioner has made steps to engage with parent, carer or child to determine and provide any early help intervention or support required but PP concerns remain around the health state and functioning of child or children.
- Inform trust Safeguarding team via email: rdash.doncastersafeguardingchildren@nhs.net.
- Practitioner to inform CAMHS consultant as the responsible consultant (RC) at this stage. Responsible consultant to consider whether the parents or carers should be informed of any concerns regarding PP.
- CAMHS consultant, with support from Safeguarding team, to request initial health information from all medical services involved with the care of the child (and siblings if appropriate).
- The trust initial health information template will be completed by the CAMHS practitioner who identified the PP concerns with support from the RDaSH safeguarding.
- CAMHS consultant to arrange a multi-professionals meeting within 28 days (or earlier) of initial identification of concerns. All health professionals involved in the child’s care and the designated professionals from ICB for safeguarding children should be invited.
- The responsible consultant will lead the meeting. Clear terms of reference and records of the meeting must be made at the time, the arrangement for these will be made by the responsible consultant.
- The Royal College of Paediatrics and Child Health (RCPCH) guidance on perplexing presentations (PP) and fabricated or induced illness (FII) in children should be followed for multi agency attendance, follow up and actions.
- All discussions and actions should be recorded in the child’s health record on the safeguarding template so that other clinicians will have access to the information. Parent and carer’s access to the record will need to be restricted, and an alert should be added to reflect this. The terminology should focus on the category of abuse or medical neglect rather than PP and FII.
Please note, if at any time a practitioner suspects or observes that a child is at immediate risk of or has suffered significant harm then a referral must be made to children’s social care as per local policy and the police.
5.1.2 Perplexing presentation concerns identified within any other trust services
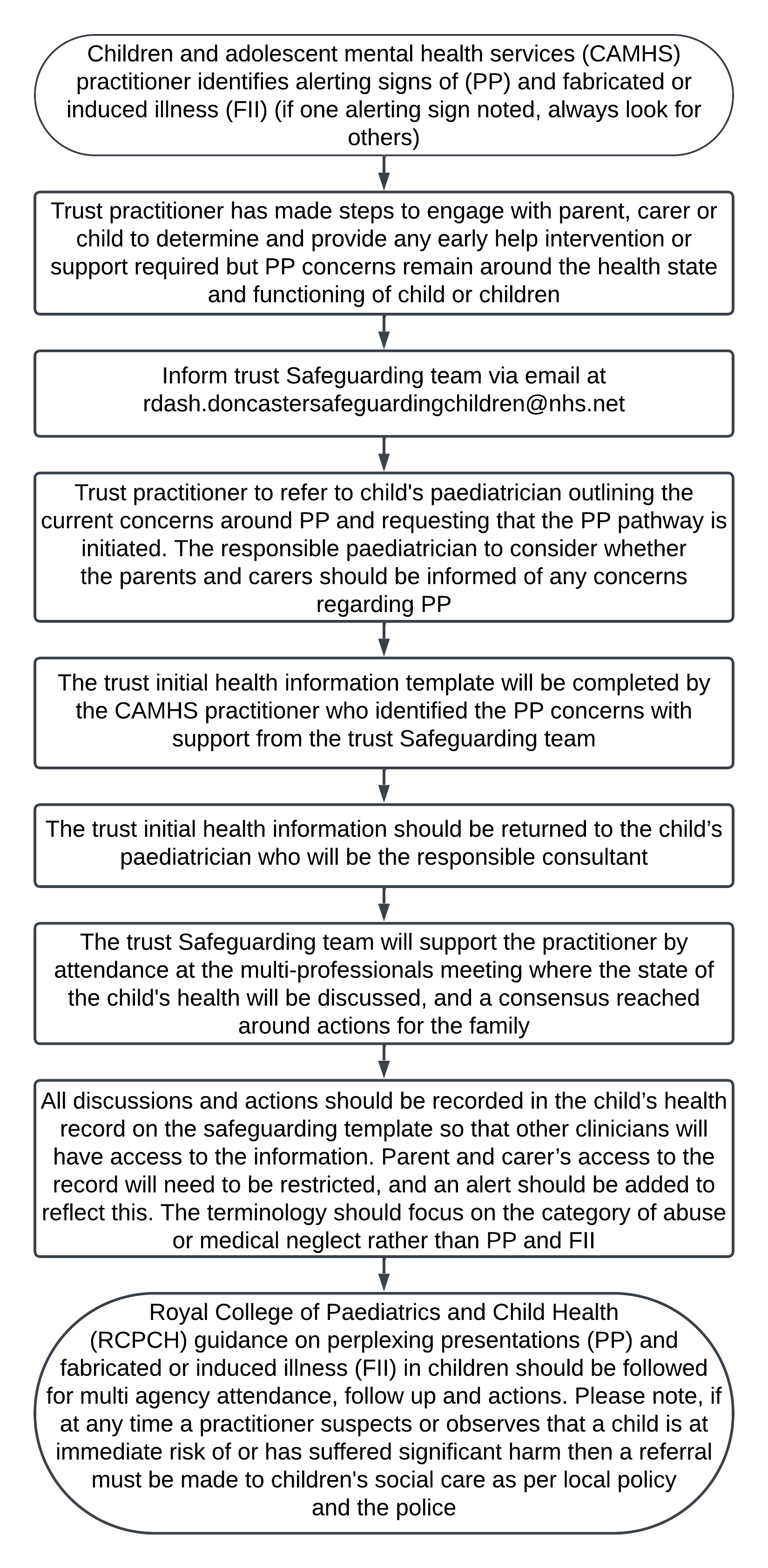
- Children and adolescent mental health services (CAMHS) practitioner identifies alerting signs of (PP) and fabricated or induced illness (FII) (if one alerting sign noted, always look for others).
- Trust practitioner has made steps to engage with parent, carer or child to determine and provide any early help intervention or support required but PP concerns remain around the health state and functioning of child or children.
- Inform trust Safeguarding team via email at rdash.doncastersafeguardingchildren@nhs.net.
- Trust practitioner to refer to child’s paediatrician outlining the current concerns around PP and requesting that the PP pathway is initiated. The responsible paediatrician to consider whether
the parents and carers should be informed of any concerns regarding PP. - The trust initial health information template will be completed by the CAMHS practitioner who identified the PP concerns with support from the trust Safeguarding team.
- The trust initial health information should be returned to the child’s paediatrician who will be the responsible consultant.
- The trust Safeguarding team will support the practitioner by attendance at the multi-professionals meeting where the state of the child’s health will be discussed, and a consensus reached around actions for the family.
- All discussions and actions should be recorded in the child’s health record on the safeguarding template so that other clinicians will have access to the information. Parent and carer’s access to the record will need to be restricted, and an alert should be added to reflect this. The terminology should focus on the category of abuse or medical neglect rather than PP and FII.
- Royal College of Paediatrics and Child Health (RCPCH) guidance on perplexing presentations (PP) and fabricated or induced illness (FII) in children should be followed for multi agency attendance, follow up and actions.
Please note, if at any time a practitioner suspects or observes that a child is at immediate risk of or has suffered significant harm then a referral must be made to children’s social care as per local policy and the police.
5.2 Appendix B Draft letter to request health information
5.3 Appendix C Health information template
5.4 Appendix D Draft referral letter
5.5 Definition of key terms
| Term | Definition |
|---|---|
| Fabricated or induced illness (FII) | A clinical situation in which a child is, or is very likely to be, harmed due to parental behaviour and action, carried out in order to convince doctors that the child’s state of physical and mental health or neurodevelopment is impaired or more impaired than is actually the case.
Synonyms:
|
| Perplexing presentations (PP) | Presence of alerting signs when the actual state of the child’s physical and mental health is not yet clear, but there is no perceived risk of immediate serious harm to the child’s physical health or life |
| Medically unexplained symptoms (MUS) | The child’s symptoms, of which the child complains, and which are genuinely experienced, are not fully explained by any known pathology but with likely underlying factors in the child (usually of a psychosocial nature), and the parents acknowledge this to be the case. The health professionals and parents work collaboratively to achieve evidence-based therapeutic work in the best interests of the child or young person. MUS can also be described as functional disorders and are abnormal bodily sensations which cause pain and disability by affecting the normal functioning of the body.
Synonyms:
|
| Responsible consultant | The responsible consultant has the responsibility for the initial management, including collating of current health involvement. This is either the CAMHS Consultant or the consultant paediatrician who has the main responsibility for the child’s care. If this is in dispute, the named doctor will liaise with the consultants involved to decide who the responsible consultant is to enable them to lead on the child safeguarding issues |
| Named doctor | A statutory role within NHS organisations, this doctor will support all activities necessary to ensure that the organisation meets its responsibilities to safeguard and protect children and young people (Safeguarding children and young people: roles and competencies for healthcare staff, published by the Royal College of Nursing in January 2019) |
| Designated professionals | Are clinical experts and strategic leaders, take a strategic, professional lead on all aspects of the health service contribution to safeguarding children across the area, providing support to all providers, and linking particularly with named child safeguarding health professionals, local authority children’s services, and local safeguarding partnerships, the safeguarding panel of the health and social care trust, and the NHS England |
| Identifying medical professional | The staff member or practitioner who has raised concerns of PP and FII |
| Professionals meeting and consensus meeting | A professionals meeting should include all health professionals involved with the child and family, including GPs, consultants, private doctors, and other significant professionals who have observations about the child, including education and children’s social care if they have already been involved. The multi-professional meeting is required in order to reach consensus about the child’s state of health |
| Health and education rehabilitation plan (HERP) | Development of the health and education rehabilitation plan requires a coordinated multidisciplinary approach and negotiation with parents and children and usually will involve their attendance as appropriate at the relevant meetings. Consideration needs to be given to what support the family require helping them to work alongside professionals to implement the plan |
Document control
- Version: 2.
- Unique reference number: 1016.
- Ratified by: Clinical policy review and approval group.
- Date ratified: 3 December 2024.
- Name of originator: Named nurse safeguarding children.
- Name of responsible individual: Executive director of nursing and allied health professionals.
- Date issued: 18 December 2024.
- Review date: 31 December 2027.
- Target audience: All clinical colleagues.
Page last reviewed: January 17, 2025
Next review due: January 17, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.
Report a problem