Contents
1 Introduction
The trust aims to provide high quality, safe and effective services for people with mental health problems, which are accessible to all who need them in line with no health without mental health. Green light for mental health (DH, 2004) and valuing people now, a three-year strategy for people with learning disabilities (DH, 2009) recommend that people with a learning disability and associated mental health problems should access main stream mental health services with specialist support from learning disabilities services where required.
This policy aims to ensure access for this patient group by working together to provide integrated care and treatment to meet the needs of people in line with current government policy and guidance.
2 Purpose
The purpose of this policy is to set out the service access pathway arrangements and care responsibilities of both learning disability and mental health services.
3 Scope
The policy applies to all adult patients with a learning disability and an associated mental health problem. The policy applies to all staff involved in the provision of services for those with a learning disability and a mental health problem. Due to the complex nature and needs of this patient group, this policy should be read in conjunction with the relevant Mental Health Act policies, Mental Capacity Act policy and the deprivation of liberty safeguards policy.
4 Responsibilities, accountabilities and duties
4.1 The board of directors
It is the duty of the board of directors to oversee that all individuals receiving care, treatment and support from the trust, receive high quality care based on an individual assessment of the range of their needs and choices. The board of directors delegates authority to the chief executive.
4.2 Chief executive
The chief executive has overall responsibility for the implementation of this policy, and in turn this responsibility is delegated to the directors and senior managers.
4.3 Medical director
The medical director is responsible for providing clinical leadership within the trust and for the provision of senior clinical advice to the board of directors. The medical director line manages the care group medical directors within each care group. The medical director is responsible for resolving issues where there are differences of opinion, which cannot be resolved by the clinical leads in adult mental health services and learning disability services.
4.4 Care group directors
Care group directors are responsible for:
- the implementation of the policy across the specified services
- the ongoing review of the policy to keep it up to date with current best practice
- providing reports to the Senior Leadership team (SLT) and the operations management meeting group (OMG) on any issues associated with the implementation of the policy
- facilitating effective joint working with internal and external partners and stakeholders
4.5 Care group medical director (consultant psychiatrist)
The role of the care group medical director is to provide advice to colleagues within mental health services and learning disability services. The role is supportive and facilitative. The care group medical director may be asked to advise and provide a second opinion for patients with complex needs where there are professional differences of opinion between services.
4.6 Non-medical consultants (for example, consultant nurse, occupational therapy consultant), allied health professionals, clinical and professional leads (or equivalent allied health professional representatives), and psychological professions leads
These staff are responsible for:
- advising the relevant care group directors in relation to service delivery requirements, staffing skills mix, staffing levels, and training needs or content of the training
- keeping up to-date with any changes to national policy or NICE guidance which may have implications for clinical practice in relation to this policy
- advising the care group directors of any changes which are required to keep practise in line with national policy or NICE guidance
- advising and supporting clinical staff when dealing with complex cases which fall under the remit of this policy
The nurse and occupation therapists consultants are responsible for:
- advising the relevant care group directors in relation to staffs training needs, and the content of the training
- keeping up to date with any changes to national policy or NICE guidance which may have implications for clinical practise in relation to this policy
- advising the care group directors of any changes which are required to keep practise in line with national policy or NICE guidance
- advising and supporting clinical staff when dealing with complex cases which fall under the remit of this policy
4.7 Service managers and modern matrons (adult mental health and learning disability)
- Service managers and modern matrons are responsible for the implementation of the policy within their areas of responsibility.
- They are the next point of escalation in cases where there are differences of opinion at team manager or at pathway meetings.
- They will ensure all relevant staff access the agreed training plan.
4.8 Community team manager and ward manager (adult mental health and learning disability)
- Community team manager and ward managers are responsible for initiating and organising the joint assessment process where it is indicated that this is required.
- The manager identifies the appropriate numbers and levels of staff and the training required for those staff to deliver safe and effective services.
- The community team manager is responsible for the appropriate allocation of patients to staff.
4.9 Clinical staff within mental health and learning disability services
It is the responsibility of all clinical staff working in these areas to:
- be familiar with, and follow the guidance as set out in this policy
- attend any training which has been identified for them in relation to this policy
- report any breaches in relation to compliance with this policy
5 Procedure and implementation
5.1 Community pathway
The trust provides both specialist learning disabilities services and mental health services (including inpatient services). Each patient should be able to access mainstream mental health services, specialist learning disability services, or a combination of both these services based on their individual needs.
Initial referrals may present in either learning disability or mental health services. It is the responsibility of the service receiving the referrals to make the initial decisions for assessment based on the protocol attached (see appendix A).
- Where both are present then a joint assessment should be undertaken, and the care plan agreed based on identified need. Where no learning disability is identified then mental health services should assess and offer treatment as appropriate. Where no mental health issues are identified, but there is a clear learning disability identified then the referral should be transferred to learning disability services. In the event of a mental health crisis, adults with a learning disability who have been identified as having additional complex needs and are at immediate risk, to themselves, or others, or harm that requires in-patient admission, staff in the Mental Health Access team should follow the guidance identified in mental health crisis pathway document for their locality (see appendix B).
- Learning disability services. Where both mental health problems and learning disability is present, then a joint assessment is to be undertaken.
- Where no significant mental health or learning disability problem is identified then the referrals should be referred onto the most appropriate service that is available.
- If referral is specifically for memory service assessment and dementia diagnostic services then joint memory service pathways have been developed and should be followed; in the first instance staff working in specialist learning disability services will initiate this process.
5.2 Details of joint working arrangements for community patients
A key objective of this policy is to facilitate more effective systems for joint working between services.
Where it is agreed that individuals who have a learning disability and identified mental health problems (dual diagnosis) require further treatment they will be placed under the care programme approach (CPA). In these circumstances, following a joint assessment, a decision is made as to which is the most appropriate service to take the lead and care coordinate, and which will act in a support or advisory role.
If adult mental health services are considered the most appropriate service to lead, then a mental health worker will be identified as the care programme approach (CPA) care coordinator, and learning disability workers will provide advice on reasonable adjustments required for people with severe and enduring mental illness who have co-existing learning disability to ensure that services and treatment meet their individual needs. They may also become co-workers delivering care planned with the person’s care coordinator under care programme approach (CPA) policy and procedures.
Where a person being cared for by the learning disability service develops a severe mental illness. If, following joint assessment, a decision is reached that adult mental health services are the most appropriate service to lead, then care co-ordination will transfer to mental health services according to the agreed care pathway. The learning disability worker would then become the co-worker and remain involved in the ongoing care of the person. There is no expectation that all care would transfer to mental health services as a result.
Adult mental health service staff will similarly provide advice to learning disability services on treatment interventions for people who have developed less severe mental health problems and who it is agreed it is appropriate to remain the responsibility of learning disabilities services.
It is essential that mainstream and specialist services work collaboratively to meet individual patient needs, utilising their respective specialist knowledge and skills to support each other in the delivery of integrated care and treatment.
The care programme approach (CPA) should be used as the framework for planning and coordinating support and treatment necessary for patients with a learning disability and mental health problems. Care plans should clearly identify the contribution of mental health and learning disability services, which will provide care coordination and which professional and Multidisciplinary team members are responsible for each component.
5.3 Care and treatment reviews
The care and treatment review (CTR) process is triggered at the point when a person is identified as ‘at risk’ of being admitted to a specialist learning disability or mental health inpatient setting. The CTR facilitates a process of seeking alternatives to admission if possible and, if not, follows them through any subsequent admission, period of assessment or treatment and towards discharge.
The aim of the CTR is to bring a person-centred and individualised approach to ensuring that the treatment and differing support needs of the person with learning disabilities and their families are met and that barriers to progress are challenged and overcome.
In the event of admission being required there should be an informal dialogue between the services consultant psychiatrists or team managers to agree which is the “most competent” service to meet the patient’s identified needs. These discussions should also take into account the commissioning arrangements and service specification and should, where possible include the views of the patient and their family.
Staff should refer to NHS England care and treatment review: policy and guidance 2015 for further guidance relating to these reviews.
5.4 Deciding which inpatient service to admit to
The decision as to where the patient being assessed as requiring a period of inpatient care is to be admitted, will be made on the basis of their primary need, and on this basis the following applies:
Learning disability primary need, individuals with significant learning disability and mental health needs who cannot appropriately be admitted to general psychiatric wards, even with the provision of additional support from learning disability services should be accessing specialist learning disability service for their mental health problems. These needs may include for example very limited communication skills (for example, verbal ability limited to use of few words and inability to speak in sentences) or significant sensory or motor impairment (mobility restricted to 50 yards or wheelchair-bound) and dependency needs for care.
Within the Rotherham and Doncaster localities any admission Monday to Friday, 9am to 5pm will be to the learning disability assessment and treatment units. Outside these hours and during bank holiday periods patients with a learning disability primary need are to be admitted to the adult mental health inpatient services and a planned admission to the learning disability unit will be facilitated at the earliest opportunity, for example, next working day.
Within the North Lincolnshire locality there is no learning disability inpatient service commissioned, so the local commissioners are responsible for sourcing an out of area placement.
There will be occasions when people with a learning disability but without a diagnosed mental illness need hospital admission in a state of crisis, either informally or under the Mental Health Act. Typically, these will be people who might previously have fallen under the (now defunct) legal category of mental impairment, and manifesting aggressive, challenging or self harming behaviour. An association with such behaviour remains a necessary precondition for the compulsory admission to hospital under a treatment order of any individual with a learning disability, for example, in the absence of any other mental disorder of a nature or degree warranting such admission.
Patients not previously known to services and who are without a formal learning disability or mental health diagnoses, if an episode of inpatient care is required these patients will be admitted to the adult mental health inpatient services for assessment. Any decision as to the need for the patient to later be transferred to the care of the learning disability services or for a shared care pathway to be implemented will be made on the basis of the assessment.
Patients with a dual diagnoses of learning disability and mental health problems, the decision as to which service these patients are to be admitted to will be based on the outcome of the care and treatment review and their primary presenting need. It needs to be recognised that this can change and any decision as to the level at which a shared care pathway is to be implemented will be determined by the patients’ current presentation.
5.5 Patients already subject to an episode of inpatient care
It is not uncommon for people with learning disabilities admitted to the assessment and treatment wards to also experience mental health problems, but usually these can be assessed and treated within the learning disability services. However if it is felt that a patient on one of the trust learning disability wards is showing evidence of more severe mental health problems a joint mental health and learning disability multidisciplinary review will be held to determine the future care of the patient, and the level and type of input required from the mental health services. In the event of the assessment showing that the patient’s primary need is in respect of their mental health problems the clinical team will need to decide if:
- the patient can remain within the learning disability service with support from a mental health worker
- due to the patients identified needs, a transfer is needed to one of the adult inpatient wards
If it is suspected that a patient on one of the adult mental health wards has an undiagnosed learning disability the clinical team are to refer the patient to the local learning disability service requesting a formal assessment and diagnosis. However formal intellectual assessment can only be completed when the individual’s level of functioning and wellbeing is at its most stable point as undertaking formal cognitive assessments when mentally unwell distorts the true level of functioning. In view of this such an assessment should be undertaken once the patient’s mental health has stabilised.
The patient is to remain under the care of the adult mental health services and a joint mental health and learning disability multidisciplinary review will be held to determine the future care of the patient, including the level and type of input required from the learning disability services. If the assessment indicates that the patient’s primary need is in respect of their learning disability a transfer to the learning disability inpatient unit or community team will need to be considered, and agreement reached as to any ongoing support required from mental health services.
5.6 Section 136 assessments
The trust has dedicated 136 assessment suites in the Doncaster, Scunthorpe, and Rotherham localities and all 136 assessments regardless of any known diagnoses will take place in these. However staff must refer to section 5.4 of this document for guidance in the event of a decision being made to admit for a period of inpatient assessment.
5.7 Providing care to patients with a diagnosed learning disability on one of the adult mental health inpatient wards
If a patient who has a mild learning disability and mental health problems can be supported via reasonable adjustments they should access the adult mental health wards. Shared care or joint working will be negotiated where issues specific to the persons learning disability have been identified. Mental health practitioners should contact the relevant learning disability services to their area to request support and advice.
The level of support required from the learning disability services will be different for each patient and determined through their individual need.
Where possible the shared care pathway is to be agreed prior to the patient’s admission and transfer and will detail:
- the frequency of contact from the learning disability services whilst the patient remains on the ward
- who will provide this contact?
- who to contact in the event of staff having any queries in respect of the patients’ learning disability needs
- who needs to be involved in discharge planning for the patient?
- when a person with learning disabilities is admitted to an adult mental health inpatient unit, the responsible clinician role will be fulfilled by the inpatient consultant. In all cases there will be liaison between the responsible clinician and other consultant colleagues involved in the care of the individual. Where an adult mental health consultant has taken the role of responsible clinician, medical responsibility will be passed back to a learning disabilities colleague when the patient is transferred back to learning disabilities services under care programme approach (CPA)
5.8 Who should be involved in agreeing the shared care pathway
The development of a shared care pathway for each individual patient is to be multi-disciplinary and involve senior clinical staff from both the trust adult mental health inpatient and learning disability services. Where possible a meeting is to take place prior to the patient being admitted or transferred to one of the adult mental health inpatient wards. In the event that it is an emergency situation the meeting should take place at the earliest opportunity following transfer and admission.
Attendance at the meeting will vary according to patient need but as a minimum it is expected that the following will be present:
- the ward managers and modern matrons (or their deputies) from the adult mental health and learning disability assessment and treatment wards
- the responsible clinicians from both services to agree responsibility
- the patients care coordinator
5.9 Risk assessment
Due to the nature of their presentation including potential risk to self and, or others all patients admitted to the adult acute mental health or learning disability wards will have a full FACE risk assessment completed. For anyone with a dual diagnosis the decision as to which module of the risk assessment to use will be based on their primary presenting need. However there may be some patients where due to their presentation it is clinically appropriate to use both the learning disability and mental health module from the FACE risk assessment tool to ensure that all potential risks are captured.
When undertaking a clinical risk assessment for any patient with a learning disability admitted to one of the adult mental health inpatient wards staff must take account of the vulnerability of the patient in such a setting as they may be more at risk of abuse or exploitation from other patients. If a patient is identified as being highly vulnerable on the adult mental health ward and steps cannot be taken to protect them for example through the use of increased nursing observation it may be more appropriate for them to be transferred to a specialist learning disability service.
As the risk assessment will inform care planning, decisions relating to leave and discharge it must be current, and reflective of the patient’s presentation, taking into account both past and present risks.
For all patients the risk assessment must be reviewed and updated as minimum:
- at admission
- weekly for all acute patients during the first month of their admission, then monthly thereafter
- prior to any periods of leave
- following periods of leave
- prior to discharge
- following any significant change to the patient’s mental state, or social circumstance
- in the event of any new and significant information becoming available
When completing the risk assessment it is important to identify the sources of information recorded.
5.10 Undertaking a mental health assessment on someone with a diagnosed learning disability
In 2010 the Royal Collage of Nursing issued their document “mental health nursing of adults with learning disabilities” which recommends that although the assessment process for someone with a learning disability will be similar it is important that:
- the assessing clinician works in partnership with the patient, their carers, support staff, and other professionals involved in the patients care
- someone is there to support the patient
- the duration of the assessment is adjusted to meet the needs and concentration span of the patient. Some may need additional time whilst for others the assessment may need to take place over a number of short meetings
- consideration is given to the fact that someone with a learning disability may become anxious during the assessment
- any communication difficulties the patient may have are taken into account, and advice sought as to what assistance the patient may need. If the patient has been assessed by speech and language therapy services a copy of their report should be sought. For some patients using pictures can help them identify their emotions
- medical jargon is avoided and words which are easy for the patient to understand are used
- any questions the patient is unable to understand are rephrased
- the assessing clinician checks the patients understanding throughout the assessment by summarising and recapping what has been covered
5.11 Additional considerations when assessing the capacity of someone with a learning disability
Staff should refer to the Mental Capacity Act policy person’s capacity is time and decision specific and based on whether the person can:
- understand the information which is relevant to the decision
- retain the information long enough to make a decision
- weigh up the information and make a choice
- communicate their decision
Timely and relevant information is key to a person being able to make a decision, and a patient can only be assessed as having or lacking capacity once they have been given the appropriate support and information to help them make the decision. As someone with learning disability might have difficulty understanding the information they will need to be supported as much as possible in the decision-making process. This support will also involve providing them with the relevant information to aid their decision-making in a format they will understand (such as pictures, symbols or audio) and allowing them enough time to process and understand the information. The following website easy health (opens in new window) provides information which may be useful.
5.12 Enhancing staffing levels
Patients with severe learning disabilities and mental health needs who are being nursed in adult mental health units may require additional dedicated support staff. If there is a need for extra staff this should be agreed at admission and reviewed under CPA. Established learning disabilities specialists from other settings should be considered, and extra staff will be accessed through the bank staff pool if necessary. Decision about extra support should not prevent inpatient staff from receiving extra training and skills development to enable them to provide safe and effective care to a patient with severe learning disabilities who has mental health needs.
5.13 Care planning
Effective care planning is dependent on good communication between the staff and patient and whilst patients with a learning disability may sometimes have significant communication needs it is essential that clinicians adapt their approach to accommodate these. If a patient has communication difficulties staff should:
- check if the person has had a speech and language therapy assessment, and if there are any recommendations that have arisen from it
- prepare appropriately for any one-on-one interactions
- use simple everyday language, and try to think of easier ways of saying a word, for example using ‘sad’ instead of ‘depressed’
- when introducing fresh information to someone use no more than two new information-carrying words in a sentence and provide an explanation, perhaps using alternative methods, to support this
- consider the use of photographs, pictures and symbols to support communication
- avoid abstract words or concepts and use concrete terms wherever possible
As far as possible the care plan must be written in terms which can be easily understood by the patient and carer where appropriate. There are tools available which staff can access to support this, some examples are:
- health action plans
- person centred support plans
- wellness recovery action plan (WRAP)
- traffic light assessment (acute health)
5.14 Patient information
As highlighted throughout this policy the type of information and the way in which it is presented to anyone with a learning disability may require tailoring to meet each patient’s individual need. Information is available in various formats and can be accessed through the trust website by clicking on the learning disability business division heading which will bring up the link to the learning disability information resource centre.
5.15 Information and support for carers or relatives
On admission it is important that clinical staff establish who the patient’s carer or relative is and if possible, the extent of the information the patient is willing to share with them about their care and treatment whilst on the ward.
Regardless of the patient’s wishes in respect of information sharing, all carers or relatives are to be given a copy of the ward carers’ pack, and where appropriate should be consulted regarding the planning of periods of leave and, or discharge from the ward.
5.16 Responsibilities in respect of any identified continuing care or specialist placement needs
Responsibility for leading the assessment and submission of any request to fund a specialist placement will rest with the inpatient service the patient is receiving care from. This will also include liaising with and keeping the patient’s identified relatives or carers informed. However if the patient is on one of the adult acute mental health wards clinical staff from the learning disability services will provide:
- support and advice as to the most suitable placement to meet the patients identified needs
- any required specialist assessments from their service
- advice around the safe transportation of the patient to the new placement
5.17 Dynamic support register
Where a person is at risk of admission to an assessment and treatment unit (ATU) or there is an imminent risk of placement breakdown a dynamic support register (DSR) application should be completed and the Crisis and Intensive Support team should be advised. Local processes should be followed in terms of ensuring the application is made on SystmOne and for ongoing monitoring of risk.
5.18 Discharge arrangements for patients on a shared care pathway
No patient on the shared care pathway should be discharged without a full multidisciplinary pre-discharge meeting with clinical representatives present from both the mental health and learning disability services. This must take place to ensure the safe discharge of the patient.
Any discharge from an episode of inpatient care will comply with the standards set out in the admission transfer and discharge policy.
5.19 Process to be followed where a difference of opinion between professionals is apparent
Wherever possible, any disagreements about the management of an initial referral, requests for case transfer or joint working should be resolved at local level, between team managers and consultants. Joint assessments may assist in resolving such disagreements.
With particularly problematic or contentious cases, it may be helpful to convene a joint planning meeting, with important decision makers from both services attending.
In the event that the difference of opinion cannot be resolved at local level the following escalation process should be followed (close and timely liaison between services is essential):
- escalate to the relevant service managers
- if the issue remains unresolved it must be swiftly escalated to the relevant care group medical directors
- the final point of escalation is to the medical director and chief operating officer, who will resolve the difference of opinion
5.20 Support for staff
It is recognised that patients who have a mental health problem and learning disability may be challenging for staff to work with, and it is therefore essential that managers:
- have effective systems in place for allocating work appropriately to staff
- have robust systems for local induction, supervision and performance and development review as per trust policy, and that appropriate training is accessed by all relevant staff
Effective working practises will be supported by:
- access to additional clinical supervision as required
- robust joint working arrangements
- use of other staff support systems such as counselling through the occupational health department
6 Training implications
6.1 All staff working in adult mental health service for example, doctors, nursing staff, social workers, allied health professionals (for example, occupational therapy (OT), physiotherapy), psychologists, support staff
- How often should this be undertaken: Once for all staff with updates as determined through any changes to the pathway.
- Length of training: Training and awareness will be delivered by a combination of:
- 3 hour learning disability awareness session.
- staff completing the learning disability education booklet.
- inclusion of specific sessions around caring for people with a learning disability and mental health problems on the staff practice development days
- Delivery method: Local induction for new starters.
- Training delivered by whom: The trusts learning and development department in conjunction with internal facilitators (including patient) and nurse and occupation therapists consultants.
- Where are the records of attendance held: Electronic staff record system (ESR).
6.2 All staff working in learning disability (LD) services for example, doctors nursing staff, social workers, allied health professionals (occupational therapy (OT), physiotherapy), psychologists, support staff
- How often should this be undertaken: Once for all staff with updates as determined through any changes to the pathway.
- Length of training: 45 minutes.
- Delivery method: Training and assessment.
- Training delivered by whom: Interagency passport module 5 Manual Handling team.
- Where are the records of attendance held: ESR.
6.3 Manual handling training, all inpatient, learning disabilities, older persons and clinical staff
- How often should this be undertaken: Annually.
- Length of training: Training and awareness will be delivered by a combination of:
- mental health first aid training
- inclusion of specific sessions around caring for people with a learning disability and mental health problems on the staff practice development days
- Delivery method: Local Induction for new starters.
- Training delivered by whom: The trusts learning and development department in conjunction with internal facilitators and Nurse and occupation therapists consultants.
- Where are the records of attendance held: Electronic staff record system (ESR).
As a trust policy, all staff need to be aware of the key points that the policy covers. Staff can be made aware through a variety of means such as:
- all user emails for urgent messages
- one to one meetings and supervision
- continuous professional development sessions
- posters
- daily email (sent Monday to Friday)
- practice development days
- group supervision
- special meetings
- intranet
- team meetings
- local induction
7 Monitoring arrangements
7.1 Implementation of the policy
- How: Baseline of current practice.
- Who by: Care group directors.
- Reported to: Implementation of the policy.
- Frequency: Baseline of current practice.
7.2 Adherence to the service access and pathway arrangements
- How: Clinical records audit.
- Who by: Adherence to the service access and pathway arrangements.
- Reported to: Clinical records audit.
- Frequency: Adherence to the service access and pathway arrangements.
7.3 Difference of opinion
- How: Clinical records audit.
- Who by: Difference of opinion.
- Reported to: Clinical records audit.
- Frequency: Difference of opinion.
7.4 Compliance with training
- How: Training records.
- Who by: Care group directors.
- Reported to: Compliance with training.
- Frequency: Training records.
8 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
8.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
Consequently, the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity, and respect, (when appropriate this should also include how same sex accommodation is provided).
8.1.1 Indicate how this will be met
No issues have been identified in relation to this policy.
8.2 Mental Capacity Act (2005)
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individual’s capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all colleagues working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason, all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected, and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 Indicate how this will be achieved
This policy will be implemented in accordance with the guiding principles of the Mental Capacity Act 2005 (section 1).
9 Associated documents
- Mental Health Act policies
- Mental Capacity Act (2005) policy
- Deprivation of liberty safeguards policy
- Care programme approach (CPA) policy
- Admission transfer and discharge policy
10 References
- Department of Health (2001) valuing people: A new strategy for learning disability in the 21st century (opens in new window).
- Department of Health (2004) green light for mental health (opens in new window).
- Department of Health (2009) New horizons.
- National service framework (1999) Department of Health (opens in new window).
- Transforming care for people with learning disabilities (2015) NHS England (opens in new window).
- Valuing people now, a three-year strategy for people with learning disabilities (2009) (opens in new window).
11 Appendices
11.1 Appendix A Adult and learning disability transition protocol
11.2 Appendix B Mental health crisis pathway, learning disabilities (LD), Doncaster, Rotherham and North Lincolnshire
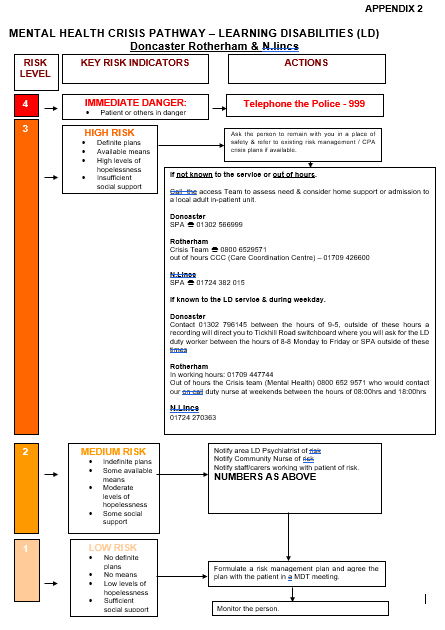
11.2.1 Risk level 4
Key indicator: Immediate danger, patient or others in danger.
Actions: Phone the police on 999.
11.2.2 Risk level 3
Key indicator: High danger:
- definite plans
- available plans
- high levels of hopelessness
- insufficient social support
Actions: Ask the person to remain with you in a place of safety and refer to existing risk management and CPA crisis plans if available.
If not known to the service or out of hours call the Access team to assess need and consider home support or admission to a local adult inpatient unit:
- Doncaster single point of access: 01302 566 999
- Rotherham: Crisis team: 08006 529 571
- Rotherham out of hours CCC (care coordination centre): 01709 426 600
- North Lincolnshire single point of access: 01724 382 015
If known to the learning disability service and during weekday:
- Doncaster, contact 01302 796145 between the hours of 9am to 5pm, outside these hours a recording will direct you to Tickhill road switchboard where you will ask for the learning disability duty worker between the hours of 8am to 8pm, Monday to Friday or SPA outside these times.
- Rotherham in working hours: 01709 447 744.
- Rotherham out of hours the Crisis team (mental health) 08006 529 571 who would contact our on call duty nurse at weekends between the hours of 8am and 6pm.
- North Lincolnshire: 01724 270 363.
11.2.3 Risk level 2
Key indicator, medium risk:
- indefinite plans
- some available means
- moderate levels of hopelessness
- some social support
Actions:
- notify area LD psychiatrist of risk
- notify community nurse of risk
- notify staff and carers working with patient of risk
- numbers as above
11.2.4 Risk level 1
Key indicator, low risk:
- no definite plans
- no means
- low levels of hopelessness
- sufficient social support
Actions:
- formulate a risk management plan and agree the plan with the patient in a MDT meeting
- monitor the person
11.3 Appendix C Mental health crisis pathway, learning disabilities (LD)
11.3.1 Who is this pathway designed to support?
Adults with a learning disability who have been identified as having additional complex needs and are at immediate risk to themselves or others or harm that requires in-patient admission.
Additional complex health needs may include significant difficulties in the following areas:
- suicidal intent
- mental illness not responding to interventions in community settings
- severe challenging behaviours
and may:
- require use of legislation
- be resistant to treatment
- be inter-related to other bio-psycho social needs
- require more than one professional and a Multi-disciplinary team to meet their needs
- require care programme approach (CPA) continued support
11.3.2 Emergency and crisis point of contact
Police: 999
- If there is an immediate risk to your safety, the safety of others or the patient, seek emergency support from the police.
11.3.3 What can patients expect?
- assessment of biopsychosocial factors and clarification of diagnosis
- risk assessment and management plans
- pharmacological and psychological based approaches
- planned discharge with a suitable care package
11.3.4 Who can refer to acute specialist learning disability services?
We have an open referral process which includes:
- GPs
- NHS clinicians
- community Learning Disability teams
- social services
11.3.5 Assessment and management of risk guidelines
11.3.5.1 Key principles
- Keep the person safe.
- Keep other people safe.
- Keep yourself safe.
11.3.5.2 Indicators of risk
Risk assessment is an ongoing process and should always be at the forefront of any practitioner’s clinical thinking. Be alert for the following:
11.3.5.2.1 Referral
- Information on suicide attempts, self-harm threats and threats to others.
- A history of depression or psychosis.
- A forensic history.
- Borderline personality disorder (BDP).
- Young men and older people are more at risk.
11.3.5.2.2 History
- Previous attempts.
- Major life changes.
- Substance misuse problems.
- Recent discharge from inpatient care.
- Serious physical illness.
11.3.5.2.3 In session factors
- Threats or plans to harm self.
- Hopelessness and no sense of a positive future.
- Current unmet need, lack of a social network and isolation.
- Mental health practitioner intuition and concern.
11.3.5.3 Proactive assessment of risk
Ask about the following:
- Level of intent: Are there definite plans?
- Degree of hopelessness?
- Problem-solving: Are there alternative ways out, possible solutions?
- Social support: Are there people at home? Can these people help?
- Access to means: Does the person have access to a means to hurt themselves?
- Harm to others: Are other people at home, carers or children at risk from the behaviour?
Document control
- Version: 8.1.
- Unique reference number: 391.
- Approved by: Clinical policies review and approval group.
- Date approved: 20 February 2024.
- Name of originator or author: Nurse consultant Doncaster care group.
- Name of responsible individual: Executive director of nursing and allied health professionals.
- Date issued: 27 February 2024.
- Review date: February 2025.
- Target audience: Staff working in or associated with learning disability and mental health services and any other staff who are involved in the implementation of this policy for example, training, audit.
Page last reviewed: February 25, 2025
Next review due: February 25, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.
Report a problem