Contents
Definitions
| Term | Definition |
|---|---|
| Preceptorship | The purpose of preceptorship is to provide a period of structured support and guidance, and development during periods of transitions for all registered practitioners that are new to trust or role |
| Preceptorship period | Between 6 and 12 months depending on practitioners’ circumstances |
| Preceptor | Person providing support and guidance to the preceptee. A qualified practitioner with a minimum of 12 months’ and had at least 12 months experience of working in the same work area as the preceptee |
| Preceptee | The new to position registered practitioner receiving support and guidance from the preceptor |
| Preceptorship lead | Central point of contact and lead for preceptorship within organisation or integrated care system (ICS) |
1 Introduction
Preceptorship will be a period of structured transition and support for:
- newly qualified practitioners
- new to area preceptees
- new to role or trust practitioners
- internationally trained practitioners
- returning to practice including returning from family leave or practitioners
Within Rotherham Doncaster and South Humber NHS Foundation Trust (RDaSH) requiring a period of support.
The preceptorship policy is for practitioners joining Rotherham Doncaster and South Humber and those changing roles within the trust and preceptors, preceptorship lead, line managers, involved directly or indirectly in the preceptorship of staff. Preceptorship is only mandatory for newly qualified practitioners and internationally recruited practitioner. Whilst it’s only mandated for those identified practitioners, all others listed above, will still have an opportunity to participate in the preceptorship programme, at the line mangers digression, if it is felt to be the best option for you during your initial supervision.
These principles form the basis of a framework and set of standards for preceptorship programme developed through NHS England (NHSE). These have been incorporated into the National Preceptorship Framework and approach.
This policy is based on the guidance and standards established by the NHSE National Preceptorship Framework (2022), Health Education England preceptorship standards (2015), the Department of Health guidance (2010). It complies with the guidance set out by the Nursing and Midwifery Council (NMC, 2020), Allied Health Professionals (2023).
The chief nurse, CEO, ICS lead, GP practice lead, board of directors of Rotherham Doncaster and South Humber organisation.
2 Purpose of preceptorship
- The purpose of preceptorship is to provide a clear Preceptorship strategy, provide support, guidance, and development for all registered practitioners to build confidence, competence and refine skills personal resilience, values, and behaviours as they transition into their new role and to continue their journey of life-long learning.
- To ensure RDaSH employees comply with local and national agreements when undertaking the role of preceptor to support preceptee’s in clinical practice.
- To ensure that there is a clear strategy and framework within RDaSH, to maintain an up-to-date register of Preceptors in all areas.
- The policy meets the requirements of the DOH Preceptorship Framework, (2010), for all registered practitioners governed by a regulatory body and Health Education England Yorkshire and the Humber recommendations (2010). This policy is based on the guidance and standards established by the NHSEI National Preceptorship Framework (2022), Health Education England preceptorship standards (2015), the Department of Health guidance (2010). It complies with the guidance set out by the Nursing and Midwifery Council (NMC, 2020). Allied Health Professional Council (AHP) 2023.
3 Scope
The preceptorship policy provides a framework and set of common standards and support (cultural, pastoral and wellbeing) which apply to all registered practitioner, nursing associates, international trained colleague, returners to practice, those returning from family leave and transitioning practitioners from one setting to another, or those colleagues requiring a period of additional support.
The preceptorship period for Rotherham Doncaster and South Humber mandates a preceptorship period for newly qualified and internationally qualified practitioners for the duration of 12 months only. For those that are either returners to practice, those returning from family Leave and transitioning practitioners from one setting to another, or those colleagues requiring a period of additional support, will participate in the preceptorship programme at your line managers digression, as it is not mandated. However, it is seen has best practice and would last for a period of up to 6 months depending on the preceptees circumstances. This will vary according to everyone’s personal progression, unless they are newly qualified or internationally trained, in which case a minimum of 12 months is required. This follows the national guidance of NHSE.
This preceptorship policy is intended as a resource for all those involved in the preceptorship of registrants within the organisation.
For more definition and information about preceptors, preceptees, please see appendix B.
4 Procedure and implementation
Line managers or recruiting managers are responsible for ensuring that the appropriate arrangements are made:
- the line manager is responsible for ensuring the new starter has attended both the trust and local induction, mandatory and statutory training, and enrolled onto the preceptee workshop where applicate as outlined above, to commence the preceptorship programme. The line manager also advises the preceptorship lead of each newly registered professional with start date and name of preceptor
- each preceptee will be allocated a nominated preceptor within the offer letter or in the first week of joining the organisation by their line manager or preceptorship lead
- the preceptee will meet with their allocated preceptor within the first two weeks of joining with the purpose of agreeing a charter and developing learning objectives for the preceptorship period
- meetings between the preceptee should take place every three months as a minimum requirement, aiming for every 2 months as gold standard. These should be documented using the standard templates (see Appendix D to I) and recorded as preceptorship supervision on the staff portal
- the line manager will support attendance and participation in all elements of the organisation’s preceptorship programme
- by the end of the preceptorship period, the preceptee will have completed their programme of learning, have developed the skills and knowledge required to ensure confidence and competence, and achieve final sign-off in their practitioner role
For some preceptees, returners to practice, new to clinical settings) an accelerated preceptorship programme (opens in new window) may be offered upon commencing the new role, however support should continue throughout the first six months, and should take into consideration performance support policy and procedure where relevant. This is for managements discretion.
4.1 Step one
- New starter accepts offer and start date agreed.
- Line manager allocates preceptor to preceptee within first week of starting new post.
- Line manager enrols new starter onto preceptee programme.
- Line manager notifies preceptorship lead of new starter and expected date of joining.
4.2 Step two
- Newly qualified or international trained practitioners has a minimum supernumerary period of 150 hours. If a longer period of supernumerary period is required, this should be negotiated by the preceptee or preceptor or equivalent or manager on an individual basis. Preceptees that are not newly qualified or internationally trained has a minimum supernumerary period of 75 hours. All supernumerary time will be reflected on the health-roster. If you require further guidance on navigating health roster (staff access only) (opens in new window)
- New starter completes trust and local induction, mandatory and statutory training.
- Preceptor and preceptee meet during first two weeks.
- Training needs analysis and SLOC (strengths, learner needs, opportunities, challenges) to be completed at initial, mid-point and final meeting.
- Individual learning plan with objectives established for preceptorship.
- Agree charter between preceptor and preceptee.
4.3 Step three
- Preceptee attends all required training and development, inclusive of the preceptee workshop followed by 3 action learning sets (this is compulsory). Preceptee’s will attend a minimum of 8 peer support or training events per year with gold standard being 12 sessions per year. See appendix N for possible topic opportunities.
- Preceptee maintains portfolio and completes reflections and relevant evidence.
- Preceptee receives clinical supervision.
- Preceptee and preceptor meet monthly, bi-monthly and quarterly.
4.4 Step four
End of preceptorship:
- Preceptee and preceptor meet for final sign-off.
- Preceptorship lead and line manager advised.
- Evaluation of preceptorship programme completed.
- Preceptee attends preceptor workshop.
- Preceptee attends the relevant student educator training for profession.
Preceptees, preceptors and managers may also utilise their specific governing body frameworks or standards if appropriate, for example The Health Professionals Council (HPC) where for example the speech and language therapist (SALT) framework may be accessed, preceptees then cross-reference to the RDaSH preceptorship programme to provide sufficient evidence to complete the multi professional preceptorship programme, this should run smoothly alongside all profession specific frameworks and not create any additional work. (refer to appendix D to I for guidance).
On completion, the preceptor and line manager must inform and share the completed exit pro forma with their local self-serve ESR administrator to input and capture this completed activity on the preceptees compliance matrix.
Please note newly qualified social workers (NQSW) who join the trust employed within RDaSH will be expected to undertake the ASYE (assessed and supported year in employment). This is an employer led 12-month programme of support and assessment, supported by the social work practice lead. Access to templates and supporting guidance is provided via skills for care. The NQSW will be responsible for completing a portfolio and will be allocated an ASYE assessor who will provide the appropriate level of supervision, undertake direct observations, and provide the appropriate reports to contribute to the ASYE portfolio.
5 Responsibilities, accountabilities and duties
5.1 The preceptor
The preceptor should be a registered professional with a minimum of 12 months experience post qualification. They should have a minimum of 12 months’ working in the work area or setting and have completed their preceptor development and workshop.
The preceptor development includes completion of the e-learning for health preceptor development programme before then completing the organisation’s 3-hour workshop (face-to-face or virtual).
The preceptor should participate in preceptorship forums and support networks to maintain up-to-date with their knowledge and will receive between 8 and 12 hours per year of protected time for preceptorship duties. A maximum of 2 preceptees per preceptor at any one time.
5.2 Role of the preceptor
The role of the preceptor is to provide guidance to the preceptee by facilitating the transition into your new role by gaining the required experience and knowledge whilst applying this understanding in the clinical setting during the preceptorship period and beyond. A minimum of 8 hours protected time is allocated to each preceptor (inclusive of training) to carry out preceptorship responsibilities to:
- plan, schedule, conduct and document regular meetings with the preceptee
- assess learning needs and develop an individual learning plan with the preceptee
- act as a role model for professional practice and socialisation
- possess a good understanding of the preceptor framework requirements and communicate these to the preceptee clearly and concisely
- act as a professional friend, peer, and advocate
- to work collaboratively with the Preceptorship Lead to ensure there are sufficient trained preceptors within each work area, to provide support and evaluate the impact of preceptorship
- participate in preceptorship forums, clinical supervision, and support networks to maintain up-to-date knowledge, including escalation process. full details in appendix C
- to provide a minimum supernumerary period of 75 hours for the preceptee
Full details can be found in appendix B.
5.3 Role of the preceptee
The preceptee is responsible for their development and commitment to their preceptorship programme. Protected time is given for all responsibilities to:
- attend all organised training and participate in all learning opportunities
- prepare for and attend meetings with their preceptor at the agreed times
- work in collaboration with their preceptor to identify, plan and achieve their learning objectives, this includes developing individual learning plan and completing all documentation within required timeframes, the guidance recommends this is added to your ongoing portfolio of development has guided by individual governing bodies
- escalate concerns, reflecting on own practice, and taking ownership of own professional development
Full details can be found in appendix B.
5.4 Role of the preceptorship lead and evaluation
The preceptorship lead is responsible for leading the programme within the trust and overseeing the preceptorship programme annually. The responsibilities of the preceptorship lead are to:
- maintain a register of preceptors and ensure there are sufficient trained preceptors
- provide development and support for preceptors
- allocate or delegate the responsibility for identifying preceptors in time for the preceptee’s start date, this is linked to the recruitment process with recruiting officers and line managers
- monitor and track completion rates for all preceptees, reported to the education and learning CLE sub on a six-monthly basis
- to work with the Workforce Systems teams to measure the effectiveness and impact of preceptorship programme on retention and staff engagement and report this on a six-monthly basis to the education and learning CLE
- measure the effectiveness and impact of preceptorship programme by completing 3 monthly audits and annual evaluations of each preceptee, including evaluation of overall preceptorship experience from preceptee feedback questionnaires at endpoint
- feedback from preceptors
- feedback from line managers, practice educators, preceptorship champions
- course evaluations
- analysis of retention statistics at 12 months and 24 months’ post registration and start date with organisation
- act as point of escalation to maintain the relationship between preceptor and preceptee
Full details can be found in appendix B.
5.5 Role of the line manager
The role of the line manager is to ensure the implementation of the preceptorship policy within own area. The responsibilities are:
- to allocate a preceptor to each preceptee within one week of their joining date
- to ensure the preceptee complete of all inductions, mandatory and statutory training applicable to their role
- to provide a minimum supernumerary period of 75 hours for the preceptee
- to work collaboratively with Preceptorship Lead to ensure there are sufficient trained preceptors within work area, to provide support and evaluate the impact of preceptorship
- to ensure the preceptee and preceptor are given protected time for meetings at the outset of programme with a meeting at minimum of every two months with a minimum of 1 hour in duration. Total of 12 to 36 hours per year in addition to attending any organisation or system programme study
5.6 Concerns
Concerns regarding the preceptor or preceptee performance must be addressed as soon as possible with the line manager. Where appropriate, escalation processes may be followed or referral to the Human Resources department or senior responsible officer (SRO).
The escalation process can be found in appendix C.
6 Programme structure
Induction and orientation to the trust and local clinical area. Attendance of the preceptee workshop and all 3 action learning sets (ALS). Support, supervision and assessment review within the clinical area through your preceptorship period. Your assigned preceptor and peer support will guide you through the process. This includes information on the education programme provided by the organisation for the preceptee. See appendix N.
6.1 Compliance
The preceptorship programme and policy should comply with:
- National Preceptorship Framework (2022)
- NMC Principles for Preceptorship (2020)
- AHP Principles for preceptorship (2023)
You may also want to refer to:
- HEE Preceptorship Standards (2015)
- Preceptorship Framework for Newly Registered Nurses, Midwives and Allied Health Professionals, DH (2010), and social workers ASYE framework.
7 Training implications
7.1 Training implications for preceptee workshop
- How often should this be undertaken: Only once.
- Length of training: 2 hours.
- Delivery method: Microsoft Teams.
- Training delivered by whom: Learning and development
- Where are the records of attendance held: Staff portal.
7.2 Training implications for action learning sets (3 sessions)
- How often should this be undertaken: All three sessions (inclusive) once only.
- Length of training: 1.5 hours.
- Delivery method: Microsoft Teams.
- Training delivered by whom: Learning and development
- Where are the records of attendance held: Staff portal.
7.2 Training implications for preceptor workshop
- How often should this be undertaken: Once only.
- Length of training: 3 hours.
- Delivery method: Microsoft Teams.
- Training delivered by whom: Learning and development
- Where are the records of attendance held: Staff portal.
8 Monitoring arrangements
See appendix A for details.
8.1 Core standards
8.1.1 Course evaluations
- How: Review and collate feedback data.
- Who by: Preceptorship lead.
- Reported to: Care group director.
- Frequency: Annually.
8.1.2 Retention statistics (12 and 24-months post registration)
- How: Review statistics at 12 and 24 months.
- Who by: Preceptorship lead.
- Reported to: Care group director.
- Frequency: Every 12 and 24 months.
8.1.3 Annual review of the programme
- How: Review, collate feedback data and complete audits of processes and supervisions.
- Who by: Preceptorship lead.
- Reported to: Care group director.
- Frequency: Annually.
8.1.4 Feedback mechanism for preceptors to support them
- How: Review and collate feedback data.
- Who by: Preceptorship lead.
- Reported to: Care group director.
- Frequency: Annually.
8.2 Gold standard
8.2.1 Session feedback
- How: Review and collate feedback data.
- Who by: Preceptorship lead.
- Reported to: Care group director.
- Frequency: Annually.
8.2.2 Feedback questionnaire on preceptorship experience, mid-point and endpoint
- How: Review and collate feedback data.
- Who by: Preceptorship lead.
- Reported to: Care group director.
- Frequency: Annually.
8.2.3 Preceptee involvement in design and development of programme
- How: Utilise feedback data.
- Who by: Preceptorship lead.
- Reported to: Care group director.
- Frequency: Annually.
8.2.4 Stakeholder feedback
- How: Review annual feedback questionnaires and audits.
- Who by: Preceptorship lead.
- Reported to: Care group director.
- Frequency: Annually.
9 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
9.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, “not just clinically but in terms of dignity and respect”.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
9.1.1 How this will be met
As a consequence RDaSH is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
9.2 Mental Capacity Act (2005)
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals’ capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, RDaSH is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
9.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the principles of the Mental Capacity Act (2005).
10 Links to any other associated documents
- Equality, diversity and inclusion
- Probation period SOP
- Disciplinary policy
- Personal development review (PDR) policy
- Supervision policy
- Corporate and local service induction policy
- Performance capability management policy and procedure
11 References
- Department of Health (2010) Preceptorship framework for newly registered nurses, midwives and allied health professionals. DOH, London.
- Health Education England (2015) Raising the bar shape of caring: A review of the future education and training of registered nurses and care assistants. HEE, London (opens in new window)
- NHS England (2022) National preceptorship model for nursing (opens in new window)
- Nursing and Midwifery Council (2006). Preceptorship guidelines. NMC Circular, London (opens in new window)
- British Dietetic Association (2021) Post registration Professional Development Framework (opens in new window)
- College of Podiatrists (2019) Clinical Career Development Preceptorship Framework. NMC (2020) Principles of preceptorship (opens in new window)
- NHS Employers (2021) Preceptorships for newly qualified staff (opens in new window)
- NMC (2020) Principles of preceptorship (opens in new window)
- Opoku, E.N., Khuabi, LA.JN. and Van Niekerk, L. (2020) Exploring the factors that affect the transition from student to health professional: an Integrative review. BMC Medical Education 21 (opens in new window)
- Royal College of Occupational Therapists (2021) Career Development Framework: Guiding principles for occupational therapy (2nd Edition) (opens in new window)
- Royal College of Speech and Language Therapy (2019) Competency Framework for Newly Qualified Practitioners (opens in new window)
- Health Education England. Allied health Professions (AHP) Preceptorship Standards (opens in new window)
- NHS England (2023) (opens in new window)
12 Appendices
12.1 Appendix A National preceptorship model
The following national preceptorship model is based on the national preceptorship framework for nursing and allied health professionals however has been adjusted to accommodate all registered practitioners.
The purpose of preceptorship is to provide support, guidance, and development for all registered practitioners to build confidence and develop confidence whilst gaining further competence as they transition into their new role as autonomous professional. Preceptorship may also be provided for registrants transitioning from one role or setting to another.
| Criteria | Core standard | Gold standard |
|---|---|---|
| Intended recipients | All newly registered practitioners and international qualified practitioners | All registered practitioners |
| Length of preceptorship programme | Minimum of 12 months for newly qualified and internationally trained practitioners, 6 months for other preceptees on joining the organisation | 12 months on joining the organisation |
| Supernumerary period | Minimum of two weeks’ supernumerary for preceptee (or equivalent to 75 hours) | Additional protected time throughout the programme for preceptor and preceptee included in preceptorship policy for organisation |
| Meeting requirements (preceptor and preceptee) | Minimum of 3 meetings:
|
As a minimum, every two months including:
|
| Roles (with expectations) |
|
|
| Preceptor |
|
|
| Preceptorship lead |
|
Plus:
|
| Core elements |
|
|
| Indicative content of development programme |
|
May include:
|
| Compliance |
|
|
| Monitoring and evaluation arrangements |
|
May include:
Recommendation of senior accountable officer at board level within organisations and ICSs. Note, where accelerated programmes are used, support should be available for six months. |
12.2 Appendix B Role descriptors
12.2.1 Preceptor role descriptor
To provide guidance to the preceptee by facilitating the transition into their new role. The role of preceptor should be provided with protected time as set out in the preceptorship policy.
- Possess a good understanding of the preceptorship framework requirements and communicate these to the preceptee clearly and concisely.
- Understand the scope and boundaries of the roles of the preceptee.
- Act as a professional friend, peer, and advocate.
- Act as role model in regard to the preceptee and maintain professional boundaries including the recognition of the social media policy.
- Ensure all induction has been completed and check that the preceptee is fully aware of local ways of working and appropriate policies.
- Facilitate introductions for the new starter to colleagues, Multidisciplinary team, peers and others (internal and external to the organisation as appropriate).
- Promote networking and development of effective working relationships.
- Complete the preceptee interviews in a timely manner relevant to specific requirements.
- Provide constructive feedback to the preceptee that fosters growth and development including the use of critical reflection.
- Use appropriate learning experiences such as carers, patients, clients, peers to meet individual learning requirements, inclusive of neurodiversity, cultural diversity and direct to the various networks we have in our trust.
- Agree learning needs with preceptee, develop a learning plan with achievable goals with regular and confidential review with the new to post practitioner.
- Use coaching and mentoring skills to enable the new practitioner to develop both clinically and professionally and to develop confidence within their new role.
- Facilitate a supportive and inclusive learning environment by signposting resources and actively planning learning opportunities for clinical, professional, and personal growth of the preceptee.
- Give timely and appropriate feedback to the preceptee on a regular basis.
- Liaise with the line manager to monitor progress and address areas of performance development or areas requiring further development through objective setting and regular review.
- Ensure own knowledge and skills are up-to-date in respect to continuing professional development and governing body requirements, which includes attending the trusts’ preceptor workshop and action learning sets, and relevant updates.
12.2.2 Preceptee role descriptor
The preceptee is responsible for their development and commitment to their preceptorship programme. The responsibilities of the preceptee are to:
- attend all organised training and participate in all leaning opportunities including induction
- prepare for and attend meetings with their preceptor at the agreed times and within the requirements of the framework
- have a clear understanding of the objectives and learning outcomes of the preceptorship framework
- work in collaboration with their preceptor to identify, plan and achieve their learning objectives, this includes developing individual learning plan and completing all documentation within required timeframes
- promote the role to a high standard
- maintain timely and professional behaviour at all times
- adhere to their individual code of professional practice
- escalate concerns, reflecting on own professional practice, and taking ownership of own development
- training requirements, include attending preceptee workshops and networking events which include peer supervision and at least 3 sessions of Action Learning Sets per year at minimum before they can be signed off
12.2.3 Preceptorship lead role descriptor
Each organisation should have an appointed preceptorship lead who is responsible for overseeing the preceptorship programme. The role may be combined with another role depending on the organisation and the number of new preceptee’s.
The responsibilities of the preceptorship lead are to:
- coordinate the identification of preceptors, knowing who they are and providing appropriate level of preparation and support
- identify all preceptee’s requiring preceptorship and others for whom preceptorship is deemed beneficial
- allocate or delegate the responsibility for identifying preceptors in time for the preceptee’s start date
- this may include involvement in the recruitment process
- monitor and track completion rates for all preceptees
- perform regular checks that the preceptor and preceptee relationship is working satisfactorily
- identify any development and support needs of preceptors
- measure the effectiveness and impact of preceptorship programmes on retention and staff engagement
- evaluate programmes after each cohort
- ensure there are sufficient trained preceptors
- support and prioritize staff retention
- act as point of escalation to maintain the relationship between preceptor and preceptee
- use coaching skills and techniques to facilitate as appropriate
- may include development of preceptorship champion network
- liaise with other local and national preceptorship leads
- ensuring preceptorship is operating within the DH framework (2010), HEE Standards (2017), NMC Principles of Preceptorship (2020) and National Preceptorship Framework (2022) Allied Health professionals’ framework (2023)
12.2.4 Preceptorship champion role descriptor
The role of the preceptorship champion may be any registered. The role of the preceptorship champion is to promote the value of preceptorship and support implementation within their area or organisation. The role should be held by an experienced preceptor who is passionate about preceptorship.
The responsibilities of the preceptorship champion are to:
- raise the profile of the preceptorship programme, the value and benefits within own clinical area or organisation.
- act as a role model for best practice in support of preceptee’s or act as a role model for best practice undertaking the preceptorship programme (this will depend on whom the champion is)
- engage with the organisation’s preceptorship team to continue the evolution of the preceptorship work internally and across region as appropriate
- liaise with other preceptorship champions and facilitate development and delivery of preceptorship communities of practice
- feedback to organisation’s preceptorship team when improvement and education is required in areas or where newly qualified staff require additional input
- share knowledge and skills with others to help them develop their thinking and practice
12.2.5 Service and team managers
Are responsible for supporting the role of the preceptorship in practice by:
- allowing preceptor’s time to complete relevant training required to support preceptees in clinical practice
- allowing preceptors one hour per week protected time to support the preceptee to develop in practice
12.3 Appendix C Escalation process
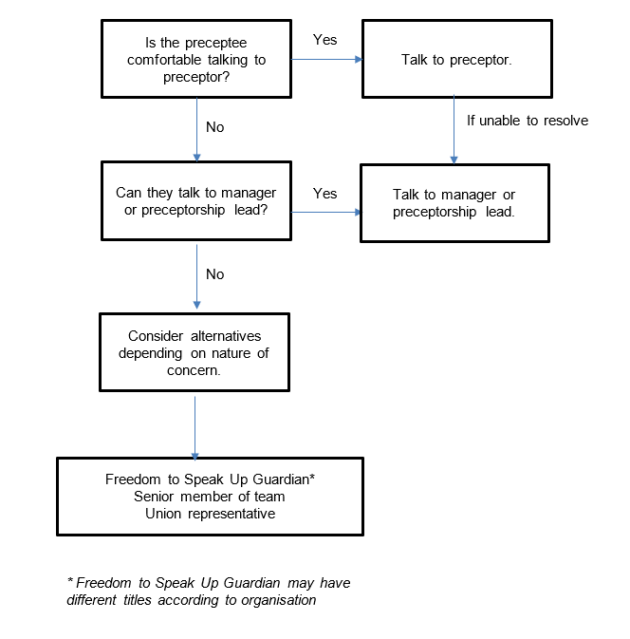
The following National Preceptorship escalation process is a sample chart to guide preceptees who have challenges.
The RCN offer comprehensive guidance on escalation process for nursing staff. This is available at raising concerns, guidance for RCN members, Royal College of Nursing (opens in new window)
RDaSH have a policy around Listening and responding to concerns and complaints policy (formally complaints handling policy) and a Respect, civility and resolution (formerly bullying and harassment) policy, these may further support this process.
12.3.1 Escalation process
- Is the preceptee comfortable talking to preceptor?
- If yes, talk to preceptor:
- if unable to resolve, talk to manager or preceptorship lead
- If no, can they talk to manager or preceptorship lead?
- if yes, talk to manager or preceptorship lead
- if no, consider alternatives depending on nature of concern. (freedom to speak up guardian, senior member of team, and union representative)
Note, freedom to speak up guardian may have different titles according to organisation.
12.4 Appendix D Charter between preceptor and preceptee
12.5 Appendix E Initial meeting template
12.6 Appendix F Strengths, learner needs, opportunities, challenges (SLOC) analysis
12.7 Appendix G Individual learning plan (ILP)
12.8 Appendix H Interim meeting template
12.9 Appendix I Final sign-off meeting
12.10 Appendix J Glossary of terms and abbreviations
| Term | Definition |
|---|---|
| Accelerated preceptorship | Intensive preceptorship programme lasting approximately six weeks |
| AHP | Allied health professional |
| CEO | Chief executive officer |
| HCPC | Health and Care Professionals Council |
| NHSE | NHS England |
| ICS | Integrated care system |
| ILP | Individual learning plan |
| NA | Nursing assistant |
| NMC | Nursing and Midwifery Council |
| NRP | Newly registered practitioner |
| Practitioner | Registered professional |
| Preceptee | Person receiving support and guidance from the preceptor, usually the newly registered practitioner |
| Preceptor | Person providing support and guidance to the preceptee |
| Preceptorship champion | Designated role to promote value of preceptorship within organisation |
| Preceptorship lead | Central point of contact and lead for preceptorship within organisation or ICS |
| Preceptorship model | Short version of the preceptorship framework |
| Preceptorship period | Designated period of support and guidance for new practitioner in 6 to 12 months post registration |
| RTW | Returner to work |
| SLOC | A training needs analysis, strengths, learning needs, opportunities and challenges |
| PLT | Placement Learning team |
| HEE | Health Education England |
12.11 Appendix K Policy version control
12.12 Appendix L Preceptor skills checklist
12.13 Appendix M Additional information
Additional Information and resources are available, with relevant RDaSH team contact details:
- PLT team email address: rdash.placementlearningteam@nhs.net
- RDaSH intranet (staff access only) (opens in new window)
- RDaSH placement learning zone (staff access only) (opens in new window)
- Accelerated preceptorship guide (opens in new window)
- Management of performance (capability) policy and procedure
- Social media (employee usage) policy
- Personal development review policy
12.14 Appendix N What to expect from your preceptorship
Here at RDASH we pride ourselves on offering a multi professional preceptorship. During your first 12 months you will be well supported by learning and development and your preceptor within your clinical areas, to enable you to gain new skills and to consolidate your knowledge in a supportive caring environment.
12.14.1 Sessions
Our sessions will be delivered through a mixture of face to face and virtual sessions, where relevant.
12.14.1.1 System skills and IT
- Introduction to ESR.
- Understanding e-roster.
12.14.1.2 Specialist care
- Palliative care.
- Respect.
- MHA and MCA.
12.14.1.3 Healthy lifestyle and quality improvement
- Diabetes management.
- Smoking awareness.
- Drug and alcohol awareness.
- Essentials in nutrition.
12.14.1.4 Understanding clinical specialities
- Physiotherapy.
- Occupational therapy.
- Health and rehab support workers and assistants.
- SALT.
- Podiatry.
- Psychologists.
- Dietetics and Nutrition.
- Orthotics.
- Social workers.
- Medical, nursing and register nurse associates.
- Art therapists.
12.14.2 Topics
Below are the topics are examples of what could be included on our programme.
12.14.2.1 Discharge planning
- Discharge planning.
12.14.2.2 Patient centred care and specialist teams
- Research awareness.
- Dysphagia and mouth care.
- Patient centred care.
- Oliver McGowan.
- Culture and diversity.
12.14.2.3 Leadership and patient safety
- Leadership and resilience.
- Action learning sets (3 sessions).
- Difficult conversations.
- Assertiveness skills and development.
- Quality improvement.
- Assessing learning and supporting others.
12.14.2.4 Professional development (PDP)
- Understanding associate place partners.
- Suitably prepared and educator training.
- Effective supervision.
- Preceptor training and workshop.
- Preceptorship completion.
12.14.2.5 Patient safety and risk management
- Understanding IR1’s and how to complete.
- What is risk management.
- Falls.
In addition to these topics, you will also receive role specific support and development within your teams and wider trust.
Document control
- Version: 2.
- Unique reference number: 575.
- Ratified by: Education and learning CLE group.
- Date ratified: 13 May 2024.
- Name of originator or author: Interim lead learning and development facilitator.
- Name of responsible individual: Director for people and organisational development.
- Date issued: 31 July 2024.
- Review date: 31 July 2027.
- Target audience: All staff involved in supporting the preceptorship programme and support of preceptees development and assessments in practice.
- Details of changes: New document. Split from the multi professional mentor and educator for pre-registration and post-registration learners policy and multi-professional preceptorship policy. To only a multi-professional preceptorship policy.
Page last reviewed: January 17, 2025
Next review due: January 17, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.