Contents
1 Introduction
The death of Connor Sparrowhawk in 2013 resulted in the ‘Mazars Report’ of December 2015 into deaths 2011 to 2015 in the Southern Health NHS Trust. The report uncovered serious concerns regarding mortality systems management
The Care Quality Commission (CQC) report “Learning, Candour and Accountability. A review of the way NHS Trusts review and investigate deaths of patients in England” 2016. It showed that in some organisations, learning from deaths was not being given sufficient priority and that valuable opportunities for improvements were missed. A trust response to this paper was authored by the Medical Director in January 2017.
The National Quality Board “National Guidance on Learning from Deaths” was published in March 2017.
The Rotherham, Doncaster and South Humber NHS Foundation (RDaSH) Trust fully supports the approach to learning from deaths. This policy sets out how the trust has responded to, and will continue to respond to, the challenge of learning from patient deaths. In addition we will make it a priority to work more closely with the families and carers of patients who have died and to ensure meaningful support and engagement with them at all stages, from the notification of the death of their loved one, involvement in the investigation process through to actions taken following on from an investigation.
2 Purpose
The purpose of this policy is to set out the trust’s expectation on how it processes, responds to and learns from deaths of patients where we are the main provider of care to that person. There is no national guidance as to what constitutes a death within scope in a trust’s activities. It is something to be determined by an individual organisation. The important point is that a trust must be explicit in its policy as to what it determines is a death within scope and develop systems and reporting around this.
Our review processes should highlight areas of good practice as well as areas of suboptimal or poor care. When mistakes happen, we need to do more to understand the possible causes and ensure we work with our partners on this.
Staff need to understand that the purpose of reviews and investigations into patient deaths is to identify areas of positive practice as well as problems in care that might have contributed to the end outcome. This will enable the trust to promote quality care interventions as well as highlighting poor care both of which are key to learning lessons in order to prevent a similar event happening again.
Our systems will ensure that we integrate with the national learning disabilities mortality review (LeDeR) programme so that the deaths of patients who have a learning disability is highlighted and automatically subjected to at least a structured judgement review as well as scrutiny from the national LeDeR process.
While a focus on process is important, everything that is done should focus on compassionate interactions with bereaved families and carers as well as the outcomes from the learning from deaths.
With this in mind the core objectives of this policy are to ensure that the trust:
- prioritises and enables meaningful engagement and compassionate support between families or carers and staff and compassionate support for families or carers that is open and transparent at all stages of the process. Families and carers should be encouraged to raise questions or share concerns about the care provided during all stages of the management of deaths process from notification of death, during the review process, and finally in seeing the lessons learned and actions taken
- identifies positive practice as well as what can be improved upon in terms of service provision both to improve patient care and ultimately to reduce the probability of an avoidable death
- maintains a standardised approach to logging, screening, reviewing, investigating and learning from deaths (LoSRIL) within the trust and that the trust receives robust assurance regarding this
- maintains the focus on engagement with partners across the local care system to:
- encourage systems for learning with other stakeholders (for example, acute trusts, clinical commissioning groups, public health, safeguarding)
- agree joint reviews where appropriate with other Health and social care providers. This would include liaison with other organisations at the relevant care groups level or executive director level to ensure that there was clarity regarding the lead responsibility for a serious incident investigation notification and where appropriate agreeing terms of reference for an investigation and lead investigator status
- promote access to and sharing of broader data or information including clinical case reviews from other providers, information systems, epidemiological information and the sharing of expertise within the law and in line with extant guidance
- Support the Northern Alliance (a group of NHS mental health trusts in the north of England) to attempt to maintain a standardised approach to logging, screening, reviewing, investigating and learning from deaths wherever possible across these trusts in order to support shared definitions, common approaches to continuous improvement, sharing data and agreeing approaches for evaluation.
2.1 Definitions or explanation of terms used
As the trust provides a wide range of clinical services across inpatient, community and within other provider organisations it can lead to a degree of confusion as to who is responsible for the logging, screening, reviewing, investigating and learning from a patient’s death (LoSRIL). This leaves the risk of a death being subject to a double and uncoordinated LoSRIL or worse still not being subject to LoSRIL at all.
All deaths which have had involvement of a RDaSH service at the time of death or which occur within 6 months of the involvement of an RDaSH service are to be logged within the trust if they fall within the scope of this policy (see sections 2.1.1 to 2.1.4). This would include those individuals where the trust had received a referral for a RDaSH service but who had not received an intervention at the time of death (for example, individuals on a waiting list).
This will be facilitated by the newly commissioned mortality module within the Ulysses reporting system which previously only managed incident reporting.
A logged death is no longer automatically regarded as an incident. It becomes an incident only if it is deemed to require a structured judgement review or a serious incident investigation (in line with the serious incident policy).
To support staff in their decision-making the trust only requires staff to log, screen, review or investigate a within scope RDaSH death either because the trust is the main provider of care as defined below or where there are specific issues which move the patient into a within scope category. However if there is any doubt staff are to contact their line manager for advice.
2.1.1 We are the main provider if at the time of death the patient was subject to
- A current episode of inpatient care within our service.
- A current episode of community treatment due to identified mental health, learning disability or substance misuse needs (including a death within IAPT services).
- An inpatient episode or community treatment package within the 6 months prior to their death (mental health and learning disability services only including IAPT).
- A referral to a RDaSH service for any of the above but where an intervention had not yet been delivered (for example, individuals who die on a waiting list).
2.1.2 Patients who meet the above criteria but are inpatients within another health care provider or custodial establishment at the time of their death:
In these circumstances the death will be reported by the organisation under whose direct care the patient was at the time of their death. That organisation will also exercise the responsibilities under duty of candour. However there will be a discussion to agree if it is to be a joint or single agency investigation (this will be determined by the cause of death) and in the case of joint investigations who the lead organisation will be. This discussion will take place at a senior level (care group triumvirate, safety and quality or executive).
2.1.3 Services provided by the trust where we are not classed as the main provider
For the following services the trust is only providing a small component of an overarching package of care and the main provider is the GP or other healthcare organisation.
- Tissue viability.
- Dietetics or speech and language therapy.
- District and community nursing including specialist nurses (for example, epilepsy).
- The drug and alcohol shared care services.
- Care home liaison.
- Acute hospital liaison.
- Doncaster physical health community physiotherapy and occupational therapy.
- Specialist Palliative Care team.
- All non CAMHS children’s services.
- Podiatry.
- Community stroke, neurology and cardiac rehabilitation services.
- Admiral nursing.
- Rotherham safer neighbourhood service.
- Doncaster Substance Misuse Hospital Liaison team.
- Doncaster learning disability hospital liaison service.
2.1.4 Exceptions where out of scope may move into scope
In addition to the above if any act or omission on the part of a member of trust staff or services from one of the clinical areas where we are not classed as the main provider is regarded as a problem in care provision then the death automatically becomes a within scope RDaSH death and should be considered within the LoSRIL process.
If the Hospital liaison team is carrying out an assessment in accident and emergency which would have previously fallen under the role of the Crisis team
If the patient is also under another core team, for example, care home liaison or frailty but also under the memory clinic
In addition to the above if any act or omission on the part of a member of trust staff or services from one of the clinical areas where we are not classed as the main provider is regarded as a ‘problem in care’ provision then the death automatically becomes a within scope RDaSH death and should be considered within the LoSRIL process.
3 Scope
This policy applies to all trust staff involved in caring for patients or have responsibility for the quality of patient care.
4 Responsibilities, accountabilities and duties
Mortality Governance is now a priority for trust boards and the March 2017 Learning from Deaths Framework places great emphasis on the importance of board leadership to ensure that learning from patient deaths becomes embedded in the organisation. Within the trust the following responsibilities, accountabilities and duties apply in relation to this policy.
4.1 Chief executive, executive trust board directors and non-executive directors
Trust boards are accountable for ensuring compliance with extant guidance which includes the national guidance on learning from deaths, alongside NHS England’s Serious Incident Framework 2015 and working towards achieving the highest standards in mortality governance. They are also responsible for ensuring quality improvement remains key by championing and supporting learning that leads to meaningful and effective actions to improve patient safety and experience, and which supports cultural change.
The trust board is required to identify an existing executive director to be the patient safety director with responsibility for the learning from deaths. Within RDaSH this is the executive medical director. Additionally a non-executive director is nominated to take responsibility for oversight of progress and act as a critical friend holding the organisation to account for its approach in learning from deaths.
Both the executive and non-executive director leads will have the capability and capacity to understand the issues affecting mortality in this trust. They will challenge where necessary, to ensure high standards in mortality governance are maintained and that the care provided to patients who die is integral to the trust’s governance and quality improvement work.
In addition to the above, all of the non–executive directors are responsible for:
- ensuring that the processes in place focus on learning and can withstand external scrutiny, by providing challenge and support
- holding the organisation to account for its approach and attitude to patient safety and that there is evident learning from all deaths
4.2 Quality committee
The quality committee is a formal subcommittee of the Board of directors. The quality committee receives assurance and provides assurance to the board of directors that the all deaths are appropriately scrutinised and investigated where necessary in keeping with trust and national guidance, with particular attention to those deaths involving a patient with a learning disability (for example, the LeDeR process). It will receive quarterly mortality reports and will receive relevant audit data in relation to systems and processes detailed within the learning from deaths policy.
It will also receive an annual mortality report highlight the key issues and learning that have resulted from mortality surveillance within the trust in the previous year
4.3 Mortality surveillance group
The mortality surveillance group meets on a monthly basis and is chaired by the executive medical director. Its key responsibilities are as follows:
- to review data in relation to trust deaths including all expected and unexpected deaths, homicides of patients currently in trust care (and in addition within a 6-month period of discharge following mental health or learning disability care) in line with the learning from deaths policy
- the group will receive assurance from the care groups and provide assurance to the quality committee and the board of directors that the all deaths are appropriately scrutinised and investigated where necessary in keeping with trust and national guidance
- to receive assurance regarding the trust performance against key performance indicators in relation to mortality management
- to engage with relevant external regional and national bodies contributing to the management and improvement of quality learning in relation to mortality management and bring in relevant knowledge and skills into the organisation both to contribute to organisation learning and to cascade into the care group governance meetings
- to receive and critique the quarterly mortality report and to recommend its consideration by subsequent quality committee and board of director meetings
- to act as the central point for the gathering of risk information relating to patient deaths
- to recommend consideration of external reviews of deaths by the Executive Management team where this is deemed appropriate.
- to review relevant policies in relation to mortality surveillance and recommend their adoption to the clinical policy review advisory group as well as providing assurance of this scrutiny to the quality committee and the board of directors
- using mortality data to identify key risk groups or situations for suicide with the aim of targeting those groups or situations more effectively and thus reducing suicide rates
- engaging with relevant external regional and national bodies contributing to the management and improvement of quality learning in relation to mortality management
- acting as the organisation’s expert advisory group in terms of scanning for and digesting national guidance and other relevant documentation
4.4 Mortality operational group
The mortality operational group is a newly formed group coinciding with the implementation of the revised learning from deaths policy.
The group will meet every 1 to 2 weeks based on annual leave and mortality demand and will be chaired by the deputy medical director or a nominated senior consultant psychiatrist.
The group has the following responsibilities:
- to review all completed mortality screens on the Ulysses system
- to review all completed multidisciplinary structured judgement reviews
- to instigate all structured judgement reviews based on an assessment of completed screening tools
- to recommend the rapid dissemination of any urgent and immediate learning stemming from the review of screening tools and noted from screening or structured judgement review tools
- to ensure that relevant assurance data is provided to the monthly mortality surveillance group
4.5 Care group directors, care group nurse directors, care group medical directors or lead consultants
The care group nurse directors have the primary operational responsibility for the following (although it is the collective responsibility of the care group leaders to ensure this within their respective care groups):
- to foster a culture of responding to the deaths of patients who die or under our care and ensure staff managing deaths have the skills and training to support the LoSRIL process
- to ensure that all within scope deaths in RDaSH are logged and screened within 72 hours of becoming aware off the death
- to support the work of those involved in a structured judgement review (SJR) or serious incident investigation
- ensure mortality forms are completed by registered professional
- to promote learning from deaths as a result of any part of the LoSRIL process and to ensure that learning is acted upon and embedded
- to ensure that all Healthcare professionals within their respective care groups acquaint themselves with this policy and understand the process for learning from deaths
4.6 Head of patient safety
The head of patient safety is responsible for ensuring that:
- any deaths screened that are determined by the mortality operational group to require a serious incident investigation are logged as incidents (IR1s) within the Ulysses reporting system and are allocated to a trained trust SI investigator as appropriate.
- that serious incidents are completed within the required timeframes
- ensuring the Ulysses reporting system is used to its full potential
4.7 Trust mortality lead
The trust mortality lead is responsible for ensuring that:
- any deaths screened that are determined by the mortality operational group to require a structured judgement review are allocated to a trained reviewer as appropriate
- that structured judgement reviews are completed within 4 weeks of determination that this part of the LoSRIL process is required
- care groups receive all the relevant information on deaths reported by their care group on a monthly basis
- care groups are aware of how to check their data on the RDaSH re-portal system and that any deaths of a patient who is currently receiving a RDaSH service or has received one within the last 6 months is screened and logged onto the Ulysses system
- data is collected and published to monitor trends in deaths, with board level oversight of this process delegated to the quality committee and the mortality surveillance group where appropriate
4.8 Safety and quality operational group
This is a group which has been set up in 2020 which meets on a monthly basis. It is chaired by the director of nursing and allied health professionals. It will receive summary reports from a number of safety and quality groups including the mortality surveillance group to ensure that there is an oversight of the main quality and safety risk in the trust and organisational learning.
5 Procedure or implementation
5.1 Responding to and learning from deaths
We know our staff work under increasing pressures to deliver safe, high quality care and that sometimes patients experience a poor quality service that is rarely due to an individual’s act or omission. The culture change required is about supporting staff to be confident in identifying what they did well and where they could do better. This requires candour, openness, honesty and a just culture.
5.2 Encouraging a learning from deaths culture
The main way in which the organisation learns from the deaths of patients in their care is through having a robust logging, screening, reviewing, investigating and learning (LoSRIL) process in place and ensuring that any emerging themes or trends are analysed, actioned and shared with the clinical staff delivering care.
Learning can occur at any stage of the mortality surveillance process. Learning could come from a single death; from an identified series of deaths (for example, within a specific locality or from a specific condition or suspected cause; or from regional or national data or guidance.
Learning should identify areas of positive practice as well as aspects of care that require improvement. Although it is important that screening and structured judgement reviews should be led by members of staff who did not play a direct role in the care of a deceased patient, involving the care groups and front line clinicians should optimise the opportunity for engagement and ‘ownership’ of any improvement activity.
Learning could result in the need for rapid dissemination of information through the organisation, a summary through the monthly mortality surveillance group or as distillation through the quarterly mortality report that is ultimately presented to the board of directors.
Learning from deaths will be incorporated into the learning from deaths annual report which will be presented to the quality committee and the trust board of directors by the executive medical director.
5.3 Data to be published by the trust every quarter
The mortality surveillance group will provide the mortality data on deaths that are within the scope of this policy which the trust is required to publish on a quarterly basis via the board of directors at the public board session.
This data is required to include the:
- total number of deaths of people falling within the scope of this policy during the quarter (with deaths of patients with learning disability specifically highlighted as per the LeDeR process)
- total number of deaths that were subject to a structured review (with deaths of patients with learning disability specifically highlighted as per the LeDeR review process)
- total number of deaths that were subject to a serious incident investigation
- deaths as a result of infections such as COVID-19
- total number of deaths thought (more than 50% likely) to have occurred as a result of a problem with care delivery (with deaths of patients with learning disability specifically highlighted from the
- themes and issues identified through structured review or serious incident investigation
- actions taken as a result of any learning and progress of action
implementation.
5.4 General process of compassionate and supportive family engagement
For the death of any patient in receipt of services from the trust staff if it meets the duty of candour criteria must comply with the being open process, and as a minimum are to undertake the actions as detailed below in sections 5.4.3 and 5.4.4. For more detailed guidance staff should refer to the trust’s being open and duty of candour policy.
Condolences are to be offered by the service regardless of the route of initial contact. If the deaths falls under the remit of the medical examiner. Family views may be sought from the medical examiner’s office.
When appropriate and with sensitivity, the family or carers should be invited to raise any concerns that they may have had about the death of their loved one. If there are any concerns raised, this will automatically be regarded as an incident and the death will be subject to at least a structured judgement review (a serious incident Investigation may also be appropriate-to be determined by the mortality operational group and the head of patient safety).
If appropriate families’ preferred method of future contact re the review is to be established. It is understood that this is a sensitive situation and that families or carers may respond differently to the death and the information offered at that initial point.
5.4.1 In relation to serious incident investigations
Preferred method of future contact re the review is to be established. It is understood that this is a sensitive situation and that families or carers may respond differently to the death and the information offered at that initial point.
In cases where the preferred method of contact is not known it should in the first instance be by letter (if an address is available) as this will allow the recipient time to consider what they wish to do.
Attempts should be made to seek details of the families or carers, for example, via the GP.
In relation to family or carers who do not acknowledge receipt of a contact letter or initially decline to be involved in a process it is recognised that sometimes newly bereaved people may not be able to make a decision at this time, so staff should offer a definite date or time when they will contact the family member or carer again to talk again about what the family member or carers want to do.
If the family or carers decide they do not want to be involved in the review process we will make it clear they can contact us at any time should their decision change; we will also offer to forward to them the summary of any findings. If the family does not want contact at all about the process or findings, this will be honoured and recorded on the Ulysses system.
When appropriate and with sensitivity, the family or carers should be invited to raise any concerns that they may have had about the death of their loved one. If there are any concerns raised, this will automatically be regarded as an incident and the death will be subject to at least a structured judgement review (a serious incident investigation may also be appropriate-to be determined by the care group triumvirate in consultation with the head of patient safety).
Where the death is to be subject to a serious incident investigation, the family or carer is to be given the opportunity to be involved in the review as an equal partner.
For any family or carer where their first or preferred language is not English staff are to refer to and follow the trust interpreters policy (provision, access and use of, for patients, service users and carers).
All contact with the family member or carer must be recorded on the electronic care record and investigation data base.
If a family member wants to seek independent legal advice then this should be respected and not seen as threatening in any way. It should not lead to an automatic involvement of legal representation on behalf of the trust. If any staff member within the trust receives a communication from a legal professional, this must be discussed with an appropriate line manager who can seek further advice from the relevant care group management team or from a relevant executive director. The Caldicott guardian can also offer advice in relation to patient confidentiality matters.
5.4.2 Family support
Families support is a key following the death of a loved one. Place bases have their own process for bereavement support led by the public health services in each locality.
Within the trust bespoke family support can be accessed from a number of agencies within the organisation. This might include the chaplaincy service, crisis service, Improving access to psychological therapies or ward-based support. This will be determined on an individual basis based on need.
If support has not been offered families should be signposted to local services for support and advice.
5.4.3 Inpatient services
Follow the standard process in 5.4.
All inpatient deaths on mental health wards will be regarded as ‘red flags’ and will be subject to at least a structured judgement review regardless of the circumstances of the death (for example, even for planned end of life care). Suspected suicides and the deaths of patients detained under the Mental Health Act 1983 (as amended 2007) will automatically result in a serious incident investigation (see serious incident policy).
All other inpatient deaths (for example, Hospice, Hawthorne, Hazel, Magnolia) will be screened but may not require structured judgement review depending on the circumstances
5.4.3 Community services
Within the community services it is likely that notification of the patient’s death will either come direct from the patient’s relative or carer or another agency such as the police or HM coroner’s office.
If the notification comes via another agency the care coordinator or another staff member who knew the patient should make contact with their relative or carer and follow the advice as above.
In the event that the service is notified of the death by another patient steps should be taken to verify the accuracy of the information prior to a call being made to the patient’s relatives or carer.
If the notification comes via the trust mortality lead (see section 4.7) the staff should follow the standard guidance in section 5.4 above bearing in mind that the family or carers may not know of the trust’s involvement in the deceased’s care especially if the patient had been discharged from RDaSH services. If there are any concerns about the sensitivity of contacting the family this must be discussed with a member of the care group triumvirate who can consult with relevant others if necessary, for example, Caldicott guardian.
It is important to bear in mind that patients have a right to confidentiality that persists after death (see section 5.6) and may have made it very clear that they did not want their families to know anything about their clinical presentation when alive (see RDaSH information governance policy for more details).
5.4.5 Duty of candour
Whilst the principles of being open are to be applied following all deaths, where the trust is the main provider of care and treatment, if the death was as a direct result of a patient safety incident (or if the incident caused the patient moderate to severe harm prior to death even if this did not relate directly to the eventual death) whilst the patient was in receipt of services or in the 6 months following discharge from services, the specific duty of candour applies.
The duty of candour will also apply if a structured judgement review concludes that the death was more likely than not to have occurred as a result of a problem in care delivery.
Staff are to refer to the trust being open policy (incorporating the duty of candour) for full details.
5.4.6 Providing written information to relatives or carers
The death of a close family member or friend is emotionally difficult, and often people do not know what they need to do or where they can go for support.
Bereavement support is commissioned and provided by each locality and led by public health departments. If support and information has not been offered families and carers should be directed to the local service provider.
5.5 How to engage meaningfully and compassionately with bereaved families and carers where a family member or carer is a patient of the service
Start by considering general guidance in section 5.4
Where a family member or carer is also in receipt of services from our trust arrangements are to be made with their care coordinator or lead clinician for them to be offered increased support. Additionally there may be circumstances where due to their level of distress they find it difficult to continue their own engagement in their treatment programme, and in these cases an offer is to be made for the transfer of their care to another provider or locality. If this offer is accepted, trust staff will make the necessary arrangements.
5.6 A patient’s right to confidentiality following death
During conversations with bereaved families or carers there will be occasions when they ask very specific questions in relation to the care and treatment their relative was receiving. Whilst in most cases this will not pose an issue, there may be circumstances where we hold sensitive information that the patient may not have wished to be shared, or where sharing of information could negatively impact on the emotional wellbeing of the family member or carer to whom it is being disclosed. In answering such questions staff need to be mindful of the fact that current extant guidance is that confidentiality obligations owed by health professionals continue even after death. Additionally the Department of Health, General Medical Council and other clinical professional bodies have long accepted that the duty of confidentiality continues beyond death and this is reflected in their extant guidance.
As each situation is unique it is not possible to provide definitive guidance to staff on what information can and cannot be shared in these circumstances. Therefore any staff member who is unsure should seek advice through the following escalation process:
- refer to the trust access to healthcare record keeping policy
- speak with their immediate line manager
- contact the trust information governance service for advice
- contact the trust Caldicott guardian
- contact the trust coroners lead if queries are related to coroners Inquests
5.7 Where the patient is under the age of 18
In the case of any death where the patient is under the age of 18 the death will be subject to the Child Death Review process 2018.
The death of person under the age of 18 is also reportable to the coroner.
The death of a person under the age of 18 will automatically lead to a Structured Judgement Review or a Serious Incident investigation following screening (as it will be identified as a red flag) if the death is determined to be a within scope RDaSH death.
5.8 Reporting deaths
As soon as the clinical service becomes aware of the death of a patient for whom we are the main provider of care details must be entered into the mortality log of the Ulysses reporting system (the first stage of the LoSRIL process) by a professionally regulated health or social care professional.
The death should be screened and logged by a professionally regulated health or social care professional of the service which provided the main RDaSH service and in conjunction with other RDaSH professionals if necessary (for example, if the patient was known to two or more services).
In addition if the death is due to unnatural causes such as suspected suicide, or as a result of some other serious incident the relevant line manager, or manager on call (if outside normal working hours) is to be notified and a STEIS completed and submitted if possible within 24 hours of the service becoming aware of the death. Staff should refer to the trust serious incident policy for full guidance.
5.9 Death of a patient with a learning disability
In the case of a death of a patient with a learning disability or autism a report also has to be made to the learning disabilities mortality review (LeDeR) programme. It does not matter whether the patient was under the care of a learning disability service at the time of the death or where the death took place within an RDaSH service.
The death of a person with a learning disability is to be notified by the ward or service manager online at the LeDeR website (opens in new window).
The death of a person with a clinical diagnosis of autism who has died on or after 1 January 2022 is to be reported via phone until the online notification system is up and running by early February 2022.
The person reporting the death will be expected to complete as much of the death notification information as possible.
Once LeDeR have the details of someone’s death, they will start the review process, which they will complete in six months. Sometimes it will not be possible to complete the review in 6 months because there might be other processes going on like a coroner’s inquest or another investigation. A LeDeR review waits until all these have happened first.
The reviewer will send the completed review to the local governance group or panel with the areas of learning, good practice and concern. The group or panel will decide on actions to take, who will take these actions
5.10 Deaths which are reportable to the coroner
Any death which meets the following criteria is also reportable to the coroner and will be actioned by the RDaSH coroners liaison service if the death has not been reported to the HM coroner by another party, for example, police.
- Suspected suicide of an inpatient.
- Deaths within 24 hours of admission to hospital (unless there is an existing arrangement with the local senior coroner, for example, within 24 hours of admission at the hospice)
- Death of a patient who is subject to detention under the Mental Health Act 1983, including patients subject to a community treatment order or subject to a deprivation of liberty safeguard or planned liberty protection safeguards. Note, this may change if proposed amendments to the Mental Health Act are accepted by the government as the use of the Mental Capacity Act will increase.
- Death of a patient under the age of 18.
- The death was due to:
- poisoning, including by an otherwise benign substance
- exposure to or contact with a toxic substance
- the use of a medicinal product, controlled drug or psychoactive substance
- violence
- trauma or injury
- neglect, including self-neglect
- the person undergoing a treatment or procedure of a medical or similar
- nature
- an injury or disease attributable to any employment held by the person
- during the person’s lifetime
- death may be linked to an accident, however long ago it happened
- the death was unnatural
Police attend all cases of unexpected deaths and will report the death and provide an immediate report for the coroner.
5.11 Structured judgement review process
The trust has adapted the Royal College of Psychiatrists Structured Judgement Review SJR) Tool (2018) which is in itself based on the structured judgement review process developed by the Royal College of Physicians, a process embedded within most acute hospitals in England. It will identify both positive and suboptimal practice.
The mortality screening tool will determine if a SJR is required. There are some red flags identified in this screening tool which will automatically lead to a SJR (or escalation to a serious incident as part of the serious incident policy). The red flags can be modified over time if national guidance requires this of if the trust believes that additional scrutiny is required if certain conditions or treatments are present. Current red flags are:
- if the family or carers have expressed a concern about the circumstances of the patient’s death
- if staff members have concerns about the circumstances of the patient’s death
- death of a mental health inpatient
- discharge from mental health inpatient services in last 1 month
- under the care of the crisis resolution and home treatment service in the 6 months prior to their death
- patient had a diagnosis of Psychosis during the last episode of care (within 6 months)
- eating disorder
- learning disability or autism
- death of a patient under 18
Only trained reviewers can use the RDaSH SJR tool built into the Ulysses reporting system. However the expectation will be that the treating team or teams will be involved when the reviewer is conducting the review wherever possible. A consultant (or senior nurse if a consultant has no role in the team providing care) should be involved as part of the multidisciplinary review. This will enable teams to ‘own’ the death and the learning process. It will minimise the risk of staff feeling that the trust is coming to conclusions about the death behind closed doors and might also help with grieving issues that staff could face.
A key task of the SJR is to determine if the death was due to a problem in care (on the balance of probabilities). This should trigger the duty of candour process and formal consideration whether a further investigation is required (see critical and major incident plan).
If the SJR process identifies “poor” or “very poor” care in any section, this will be considered by the weekly mortality operational group when they review all completed SJRs.
If it is concluded that a full serious incident investigation needs to be undertaken at any stage of the SJR process, a STEIS is to be immediately completed and submitted by the trust Patient Safety team. The investigation will then follow the serious incident process and timeframes.
5.12 Governance process
The following governance framework is in place to oversee how the trust reviews and learns from patient deaths.
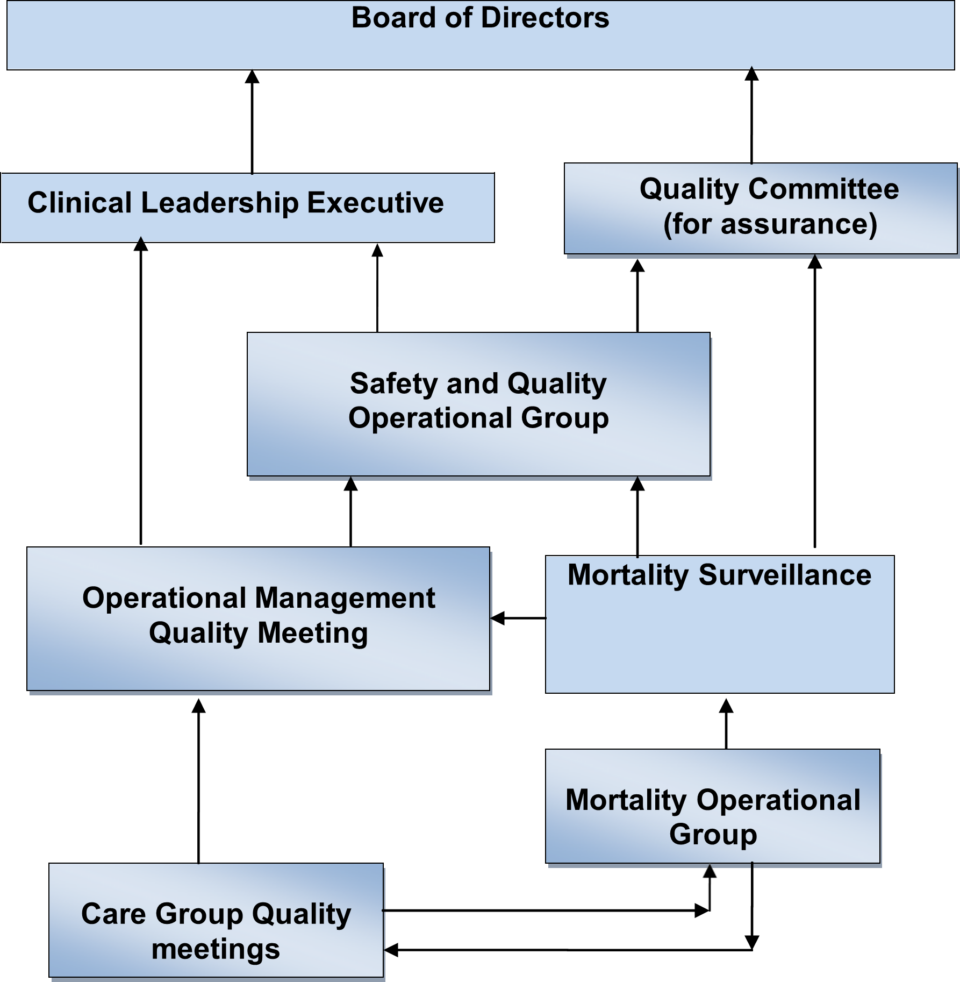
The above diagram demonstrates the Pathways for information flow and for assurance within the organisation. Operational management group support the chief operating officer in delivering the operational requirements of the trust overseen by the clinical leadership Executive. The board of directors gains its assurance directly from reports every quarter that come via the quality committee and the executive medical director regarding adherence to the learning from deaths policy.
6 Training implications
All team leaders, care group medical directors, care group nurse directors and care group directors will need to be familiar with the logging, screening, reviewing, investigation and learning systems (LoSRIL) which form the learning from deaths process.
All staff members who may be required to play a role in the LoSRIL process are expected to pay due regard to this policy. It is the responsibility of their line managers to ensure that staff understand how to log and screen deaths where appropriate.
All members of staff who undertake a structured judgement review must have been trained in this methodology.
7 Monitoring arrangements
All completed screening tools and structured judgement reviews will be reviewed by the weekly mortality operational group for assurance and a review of learning.
Internal audit (360 Assurance) conducted the first audit of the learning from deaths systems and processes within the trust in 2018. The second internal audit was submitted to the trust in February 2020. Further internal audit work and RDaSH audit activity will be negotiated after the trust completes actions in response to second internal audit report.
Key performance indicators are as follows and will be reported in the quarterly mortality report that is received by the quality committee and which then provides assurance to the board of directors:
| Action | Primary responsibility | Timescales |
|---|---|---|
| Review national spine data for newly deceased patients |
Care groups can now access their own spine data via the trust re-portal system | Weekly or monthly |
| Patient death logged on Ulysses mortality module | Professional registered health or social care professional | Within 72 hours of notification of death being received |
| Mortality screening forms reviewed |
Mortality operational group |
1 to 2 weekly |
| Structured judgement review (SJR) |
Trained reviewer with the multi-disciplinary team |
4 weeks |
| Mortality report produced |
Trust mortality lead | Monthly |
| Serious incident investigation | Lead investigator | 60 days |
| Lessons learnt presented at mortality surveillance group |
Trust mortality lead | Monthly |
| Quarterly mortality report | Trust mortality lead, presented by executive medical director | Quarterly |
| Annual mortality report |
Trust mortality Lead, presented by executive medical director | Annually |
8 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
8.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, “not just clinically but in terms of dignity and respect”.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
8.1.1 How this will be met
All identified issues in relation to the impact of this policy on the privacy; dignity and respect of patients have been addressed within the policy.
8.2 Mental Capacity Act (2005)
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals’ capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act (2005) (section 1).
9 Links to any other associated documents
- Being open policy (incorporating the duty of candour)
- Interpreters policy (provision, access and use of, for patients, service users and carers)
- Incident management policy
- National quality board (2017). National Guidance on Learning from Deaths: A Framework for NHS Trusts and Foundation Trusts on identifying, Reporting, Investigating and Learning from Deaths in Care (opens in new window)
- NHS Improvement. National Guidance on Learning from Death: Information and resources for trust boards (opens in new window)
10 Appendices
10.1 Appendix A Mortality reporting and review process
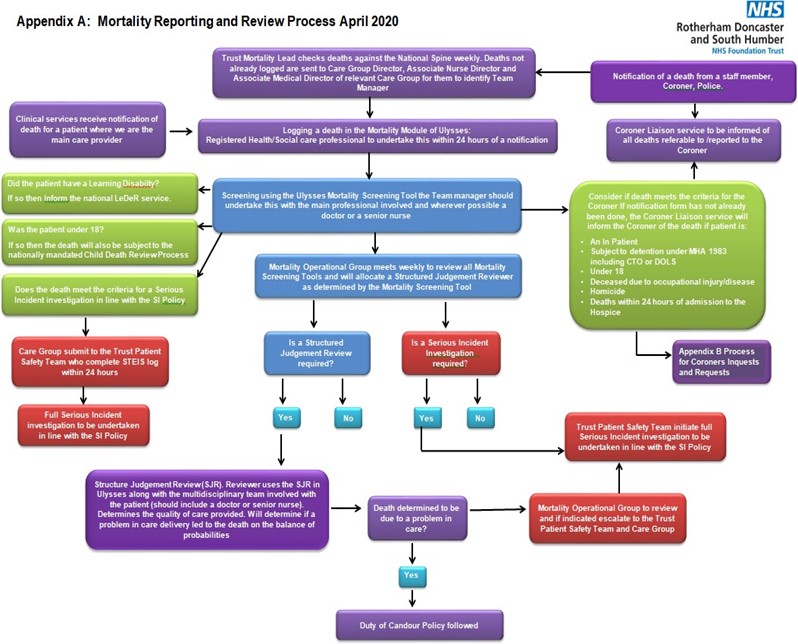
10.1.1 Initial report
Either:
- Notification of a death from a staff member, coroner, police. Coroner liaison service to be informed of all deaths referable to, reported to the coroner. Trust mortality lead checks death against the National Spine weekly. Deaths not already logged are sent to care group director, associate nurse director and associate medical directors of relevant care group for them to identify team manager.
- Clinical services receive notification of death for a patient where we are the main care provider.
Logging a death in the Mortality Module of Ulysses:
- registered health or social care professionals to undertake this within 24 hours of a notification
10.1.2 After logging
Screening using the Ulysses mortality screen tool the team manager should undertake this with the main professional involved and wherever possible a doctor or a senior nurse.
Did the patient have a learning disability?
- If so then inform the national LeDeR service.
Was the patient under 18?
- If so then the death will also be subject to the nationally mandated child death review process.
Does the death meet the criteria for a serious incident investigation in line with the serious incidents policy?
- If so care group submit to the trust Patient Safety team who complete STEIS log within 24 hours.
- Full serious incident investigation to be undertaken in line with the serious incidents policy.
Consider if death meets the criteria for the coroner if notification form has not been already done, the coroner liaison service will inform the coroner of the death if the patient is:
- an inpatient
- subject to detention under MHA 1983 including CTO or DOLS
- under 18
- deceased due to occupational injury or disease
- homicide
- deaths within 24 hours of admission to the hospice
Refer to appendix B process for coroners inquests and requests.
10.1.3 Mortality operational group meeting
Mortality operational group meets week to review all mortality screening tools and will allocate a structured judgement reviewer as determined by the mortality screening tool.
10.1.3.1 Is a structured judgement review required?
- If so, structured judgement review (SJR). Reviewers uses the SJR in Ulyssess along with the multidisciplinary team involved with the patient (should include a doctor or senior nurse). Determines the quality of care provided. Will determine if a problem in care delivery led to the death on the balance of probabilities.
Death determined to be due to a problem in care?
- Duty of Candour policy followed.
Mortality operational group to review and if indicated escalated to the trust Patient Safety team and care group.
Trust patient safety team initiate full serious incident investigation to be undertaken in line with the serious incidents policy.
10.1.3.2 Is a serious incidents investigation required?
If yes, trust patient safety team initiate full serious incident investigation to be undertaken in line with the serious incidents policy.
10.2 Appendix B Process for coroner Information or process for coroner statement requests and Inquest (referred to in appendix A)
10.2.1 Process for coroner information
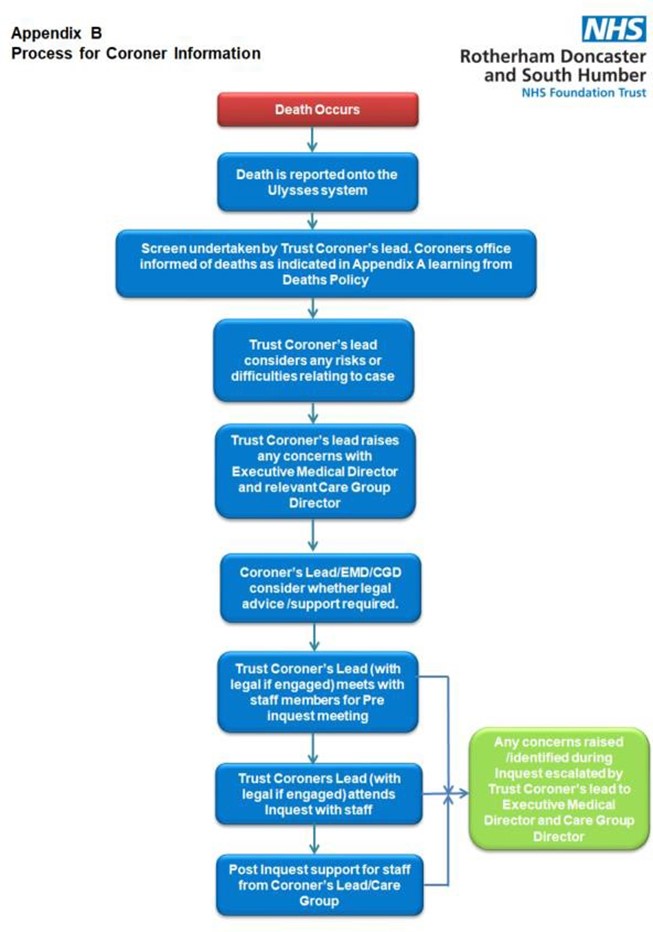
- Death occurs.
- Death is reported on the Ulyssess system.
- Screen undertaken by trust coroner’s lead. Coroners office informed of deaths as indicated in appendix A learning from death policy.
- Trust coroner’s lead considers any risks or difficulties relating to case.
- Trust coroner’s lead raises any concerns with executive medical director and relevant care group director.
- Coroner’s lead or EMD or CGD consider whether legal advice or support is required.
- Trust coroner’s lead (with legal if engaged) meets with staff members for pre-inquest meeting.
- Trust coroners lead (with legal if engaged) attends inquests with staff
- Post inquests support for staff from coroner’s lead or care group.
- Any concerns raised or identified during inquest escalated by trust coroner’s lead to executive medical director and care group director.
10.2.2 Process for coroner statement requests and inquest
- Enquiry received from the coroner to RDaSH coroner email rdash.coroner-liaison@nhs.net.
- Records review by trust coroner’s liaison service.
- Response to coroner’s office by trust coroner’s liaison service.
- Request for report from coroner’s office to chief executive’s office.
- Request forwarded to corner’s liaison service.
- Trust coroner’s lead request statement from staff via service manager or care group triumvirate.
- Report review by executive medical director, doctors, trust coroner’s lead, staff.
- Report submission to the coroner by trust coroner’s liaison service.
10.3 Appendix C Additional Process if death is COVID-19 related
10.3.1 Overview
NHS England or NHS Improvement published on the 23 March 2020 guidance outlining details of a new central electronic notification system for any death of an inpatient with confirmed COVID-19, the COVID-19 patient notification system (CPNS). Note, GPs will report any community death.
10.3.2 RDaSH response, operating procedure
The existing processes outlined in policy and procedure will remain relevant for any COVID-19 related deaths (at this present time until any point where any guidance indicating otherwise is published). This includes criteria on expected or unexpected deaths and processes, and expectations to report the death within 24 hours. Policies or procedures already exist for care of the adult patient following death, verification of expected death policy; and learning from deaths. Attached at appendix A is the process flow which outlines notification, reporting and management of deaths as an over-arching aid.
10.3.3 Roles and responsibilities
Registered professionals responsible for reporting deaths would be maintained for COVID-19 related deaths. These will be the care group triumvirates, modern matrons and supported by the trust lead for mortality, inquests and suicide prevention and the nurse consultant in the hospice. The registered professional responsible for logging any death will also take personal responsibility to make contact with the regional single point of contact for any patient where the NHS number is unknown in order to ascertain a unique reference number, essential for reporting purposes.
10.3.4 National COVID-19 patient notification system (CPNS)
National guidance is available to support the use of this system for the registration of COVID-19 related deaths.
10.3.5 RDaSH reporting
Deaths will continue to be reported onto the trust mortality reporting system. This will continue to be in accordance with the trust Learning from Deaths policy that describes a within scope death. A COVID-19 patient could die in a non RDaSH setting (meaning no national CPNS notification from RDaSH) but might still require their death logging and screening within the trust Ulysses mortality module if it is a within scope death, for example, community LD team, Early intervention in psychosis, substance misuse patient.
The narrative in the mortality module includes specific information required in relation to COVID-19 in scope deaths. These deaths include:
- where the death was due to confirmed or suspected COVID-19 (where swab result has been completed and results obtained or awaited)
- where COVID-19 is identified as a direct or an underlying cause of death on the death certificate (even if the screening test was negative or had not been taken prior to death)
- where the death is that of an RDaSH staff member or volunteer
10.3.6 Reporting a COVID-19 death on Ulysses mortality system
The Ulysses system has been updated to include a number of domains required for data capture. These include:
- whether the death was due to a confirmed case of COVID-19 (swab obtained before death)
- whether the death was due to a suspected case of COVID-19 (swab sent before death) For the above please include in the narrative the date the swab was sent and the date received
- where COVID-19 was identified as an underlying cause on the death certificate We have an additional requirement to log any staff or volunteer deaths. This is further separated into
- deaths in a RDaSH in pt bed
- death in a non RDaSH bed
- death in the community of a RDaSH patient When logging a death please ensure that the location of the death is clearly documented

If you have any queries please contact either:
- Sharon Greensill: s.greensill@nhs.net
- Natasha Collinson: natasha.collinson@nhs.net
Document control
- Version: 4.1.
- Unique reference number: 447.
- Approved by: Board of directors.
- Date approved: 21 February 2024.
- Name of originator or author: Executive medical director.
- Name of responsible individual: Executive medical director.
- Date issued: 5 March 2024.
- Review date: March 2024.
- Target audience: Clinical staff in all services across the trust.
Page last reviewed: November 15, 2024
Next review due: November 15, 2025
Problem with this page?
Please tell us about any problems you have found with this web page.