Contents
1 Introduction
The provision of clean linen is a fundamental requirement for service user care. Incorrect handling or processing of linen can present an infection risk to all colleagues who process and handle laundry items and to the service users who subsequently use them.
Although linen may become contaminated with body fluids, which carry the risk of infection, there is in fact a minimal risk to others if correct procedures are followed.
The contents of this policy are based on the “Choice Framework for Local Policies and Procedures 01 to 04: Decontamination of Linen for Health and Social Care: Management and Provision Manual, Version 1” (CFPP01-04) This policy should also be read in conjunction with other trust infection control policies, including but not limited to:
- hand hygiene policy
- decontamination policy
- isolation policy
2 Purpose
The purpose of this policy is to set out the procedures which must be taken to minimise the risk of infection by making colleagues aware of the correct procedures for categorisation, segregation, transportation and handling of linen so that the risk of potential cross-infection is minimised.
2.1 Definitions or explanation of terms used
The definition of linen for the purposes of this policy includes sheets, pillow cases, towels, duvet covers, blankets, counterpanes and patient clothing.
2.1.1 Categories of hospital linen
- Clean and unused linen, linen that has not been used since it was last laundered.
- Used linen, all used linen not classified as contaminated.
- Foul or infected linen:
- foul soiled with body fluids including urine, blood, vomit, or poo
- infected known infected linen
This system of categorisation applies when either the items are being laundered at the trust’s Tickhill Road Site laundry or by laundry contractors (where applicable).
3 Scope
This policy is applicable to all colleagues and managers or supervisors of colleagues who in the course of their work will be involved in the handling, transportation, labelling, washing and processing of linen and, where applicable, patients clothing.
4 Responsibilities, accountabilities and duties
4.1 Care group directors or care group nurse directors or deputy care group directors or service managers or supervisors
It is the responsibility of managers and supervisors to make their colleagues aware of this policy in order to promote good practice and therefore reduce the risk of infection from the handling, transporting and laundering of linen.
4.2 All staff involved in the handling, transportation, labelling, washing and processing of linen
It is the responsibility of colleagues involved in the handling, transportation, labelling, washing and processing of linen to:
- follow the procedures set out in this policy
- be aware of and follow the relevant local procedures for their specific locations or geographical areas of work
- categorise, segregate and dispose of linen as per this policy
- be accountable for their own practice and always act to promote and safeguard patients, colleagues and visitors from the potential risk of cross infection from used linen
- ensure all patient clothing, curtains, hoist slings and slide sheets are clearly labelled before putting into the laundry system
4.3 Laundry colleagues
It is the responsibility of laundry colleagues to:
- take personal responsibility for wearing personal protective clothing when handling all used, soiled and contaminated linen. Refer to the personal protective equipment policy
- ensure that red water-soluble bags are placed unopened into the washing machine
- record wash temperatures for every wash cycle and retain completed temperature logs for 6 months. Any abnormal readings must be reported to the estates department immediately for corrective action to be taken
5 Procedure or implementation
5.1 Inpatient areas
The storage of clean linen:
- when not in use, clean linen must be stored above floor level, in a designated linen cupboard with the door closed or an appropriate identified covered trolley to minimise the risk of contamination from dust
- clean linen must never be stored within the bathroom or sluice
- if clean linen is taken into an isolation area and not used the linen must be laundered again before storage or use
- any torn, damaged or stained linen should be placed in a clear plastic bag and returned to the laundry. The bag should be labelled showing the place of origin and the reason for return
- linen storage facilities must be kept clean, this includes cupboard shelves, floor coverings and wheels of the linen cages
- linen storage facilities are to be used for the storage of clean linen items only and not used for storage of any other equipment (for example, Christmas decorations, single use bedpans or urinals.)
Holding and storage of used linen (including contaminated linen):
- all used linen must be handled with care to minimise the transmission of micro-organisms via dust and skin scales. Disposable aprons must be worn when there is a risk of contamination to and from colleagues clothing when making or changing bed linen
- infected or foul linen may contain potential pathogens and therefore should be removed from the bed with care and placed immediately into a red water soluble bag at the bedside and then directly into the designated green wheelie bin. It must not be placed on the floor or carried through the ward or department
- care must be taken to remove any extraneous items from used linen before it is placed ready for laundering. Such items are potentially dangerous for colleagues handling the linen and may also damage laundry equipment
- used linen awaiting collection must be stored in a secure area away from public access and in the secured wheelie bin. Care should be taken to ensure the wheelie bin is not over filled and that the lid can be fully closed
- green wheelie bins must be secured with a ward identifiable tie wrap in accordance with the protocol outlined in appendix A
5.2 Transportation of linen
- Clean and dirty linen must not be transported together unless impervious barriers are in place.
- Used laundry items must not be decanted from one wheelie bin to another for the purposes of transportation. Such practice will present a significant risk to colleagues breaching the policy.
- Logistics colleagues must follow their departmental ‘standard operating procedures for cleaning or decontamination of vehicles’ for any vehicle which is used for transporting used or contaminated linen.
5.3 Advice to staff on the laundering of uniforms
- Uniforms must be changed daily.
- Where the service is available it is recommended that colleagues send their uniforms to the laundry.
- If uniforms are washed at the individual’s home, they must be washed separately from other items and on a machine cycle that reaches 71C (for not less than 3 minutes) or 65C (for not less than 10 minutes). Therefore, it is important that when uniforms are being purchased, they can withstand laundering at 65C.
- If a uniform becomes contaminated with blood or body fluids, it must be changed for a clean one as soon as possible. The contaminated item must be placed in a red soluble bag. Ideally it should be sent to the laundry (if this service is applicable) rather than taken home.
- The above principles also apply to the laundering of healthcare workers own clothing if worn for clinical work. Therefore, clothing should be worn that can withstand the above laundering temperatures.
5.4 Advice to colleagues on the laundering of patients clothing on ward areas
- All personal items of clothing that cannot be taken home by visitors or relatives should be laundered by the trust’s laundry. For patients on a rehabilitation ward, the laundering of clothing can be undertaken in the appropriate designated area within the clinical area.
- All patient clothing which is to be sent for laundering must be labelled with the patient and ward location. It is the responsibility of ward staff to ensure all patient clothing is clearly labelled.
- All patient clothing sent to the laundry must be placed in a green patient clothing bag in line with the procedure in appendix A.
- Delicate garments, hand wash only, dry clean only or any other personal items that may need special wash treatments should be discouraged as these items cannot be safely decontaminated without the risk of damage. These items should not be sent to the trust’s laundry as they may be damaged in the washing process. Where possible, check the garments label for any special wash instructions.
- Patient clothing that is known to be infected or foul must be placed in a red water-soluble bag for use in domestic machines. Seek advice from the laundry to ensure the correct bags are being used. These bags are different to the red water-soluble bags used for hospital linen.
- Manual sluicing and soaking of soiled laundry must never be carried out, even if the item is to be taken home by the visitors or relatives. A machine sluice cycle or cold prewash must be used for all soiled items. Care should always be taken not to overfill the washing machine drum.
- Heat-resistant items must be processed in a cycle which reaches 71C (for not less than 3 minutes) or 65C (for not less than 10 minutes).
- Heat labile items should be washed on the hottest cycle possible for that item.
- Inpatient areas who are considering procuring a new or replacement washing machine or drier, must contact the Estates department for advice on machine type or capability.
- If there are any plans to change the fabric, fixtures or fittings of the designated laundry room, the Infection Prevention and Control team must be informed at the earliest opportunity to ensure the changes meet IPC standards.
5.5 Advice for relatives or carers who take patients clothing home to wash
- Used or dirty clothing may be stored in the patient’s locker or wardrobe or sluice area for a short period only. If clothing is soiled with body fluids and has an odour it may be more appropriate to store these items in an appropriate bag in the sluice areas. The bag, in turn, should be labelled with the patients name and placed in a cleanable, lidded receptacle. Ideally relatives should be taking used clothing home daily.
- Solids must be removed from any garments and disposed of appropriately. The clothing should then be placed in a patient specific water-soluble bag and secured according to manufacturer’s instructions. Red water-soluble bags used in clinical areas must not be used to store clothing that is being laundered by relatives or carers as they cannot be placed in domestic washing machines. If used in a domestic machine they may cause damage and render the machine faulty
- Infected or foul clothing must never be manually sluiced. Relatives or carers should be informed of the type of soiling (if appropriate) and advised regarding the safe handling of contaminated linen.
- If clothing is grossly contaminated or soiled it should be discussed with relatives or carers that the safest means of decontaminating the clothing would be to send it to the hospital laundry. It must be emphasised that there is a risk that the items may be damaged during the washing process due to the high temperatures required to render the item of clothing safe. The laundry will not be held liable for any damage to such items. If the clothing is not labelled with the patient’s name the laundry colleagues will need informing prior to the clothing being sent
- For infected or foul clothing, protective gloves should be worn (for example, household rubber gloves) to handle the clothing. Items must be placed directly into the washing machine. The gloves should be washed and dried and used for that task only. Hands should then be washed thoroughly.
- If soiled with body fluids, the relatives or carers should be strongly advised that a pre-wash or sluice cycle should be used prior to the main wash. Clothing should be washed at the hottest possible temperature the fabric will withstand. The clothing should not be washed with other household members clothing.
- For used clothing (not soiled) garments can be placed in a green patient clothing bag for ease of transportation and then the items can be placed into the washing machine and wash at the hottest temperature the fabric will withstand. Relatives should wash hands thoroughly after handling items.
5.6 Manual handling equipment
Patients should have their own hoist sling or slide sheet (where required) whilst receiving inpatient care. Once the patient has been discharged the sling or slide sheet is to be laundered in the trust’s laundry. Where there is any soiling of fabric items, they must be laundered immediately and are not to be washed by hand in the ward area.
All hoist slings or slide sheets should be clearly marked with the ward name.
5.7 Waterproof pillows and duvets
Waterproof pillows and duvets must not be sent to the laundry for laundering. All pillows and duvets must be covered by an impervious waterproof cover with welded not stitched seams. If the pillow or duvet becomes soiled or damaged, it must be discarded and recorded as condemned by the ward.
All pillows and duvets must be marked with the ward or area name in permanent marker pen.
All pillows and duvets are to be cleaned by hand at ward level using the appropriate disposable cleaning wipe, in line with manufacturer instructions.
5.8 Curtains and soft furnishings
Curtains in clinical areas must be laundered routinely on a six monthly basis or sooner if they become visibly soiled or have been on an area with a known infection. Any curtains purchased for clinical areas must be machine washable or be of the disposable type. Curtains must be labelled indicating when the next six monthly routine cleans should take place.
For curtains coming from a ward area which has had a known infection or outbreak, a member of the ward team is advised to contact the laundry prior to removing the curtains for advice on laundering procedures. Curtains from an infected area which are placed in a red dissolvable bag will be laundered at high temperatures which may result in shrinkage to some fabric types.
Within clinical areas soft furnishings, such as chairs, must be purchased with wipe clean, fluid repellent upholstery, advice should be sought from the Infection Prevention and Control team. Any chairs that become stained or soiled must be steam cleaned or discarded as soon as possible.
5.9 Mop heads
Reusable mop heads must be machine washed on a daily basis, separately from other items, by the trust’s laundry. Used mop heads should be placed in a red soluble bag and placed into a wheelie bin identified for the collection of other infected items contained within red soluble bags.
5.10 Containment of infected or foul linen items
The use of red soluble bags to contain infected or foul linen items is vital to minimise the risk of infection. These are easily available from the laundry by calling 03000 214014.
If infected or foul linen items are not contained securely on arrival at the laundry the originating area will be contacted and asked to attend the laundry department to deal with and render safe any items. An incident form will be completed by laundry personnel following any such occurrence.
6 Training Implications
Staff will receive instructions and direction regarding infection prevention and control practice and information from a number of sources:
6.1 All staff and managers of staff who in the course of their work will be involved in the handling, transportation, labelling, washing and processing linen and, where applicable, patients clothing
- How often should this be undertaken: Once.
- Length of training: 1 to 2 hours.
- Delivery method: Local induction.
- Training delivered by whom: Peer or manager.
- Where are the records of attendance held: Personnel file.
As a trust policy, all colleagues need to be aware of the key points that the policy covers. Colleagues can be made aware through:
- trust policies and procedures available on the intranet
- ward or department line managers
- trust infection prevention and control teams
7 Monitoring arrangements
7.1 Storage of soiled or contaminated linen
- How: Daily linen processes.
- Who: Laundry personnel.
- Reported to: Laundry supervisor or IR1.
- Frequency: Daily.
7.2 Wash temperatures of main hospital laundry
- How: Daily laundry processes.
- Who: Laundry supervisor.
- Reported to: Records held for 6 months. Any faults reported to estates for repair.
- Frequency: Daily.
7.3 Storage of clean linen
- How: Facilities Monitoring audit exercise.
- Who: Facilities monitoring officer.
- Reported to: Head of Facilities or matrons or sisters or IPC.
- Frequency: Varies dependent on risk category of area (between 1 and 3 months).
8 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
8.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
8.1.1 How this will be met
No issues have been identified in relation to this policy.
8.2 Mental Capacity Act 2005
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals’ capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all colleagues working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act (2005) (section 1).
9 Links to any associated documents
- Choice framework for local policies and procedures 01-04: Decontamination of linen for health and social care. Management and provision manual. Consultation draft 22 July 2011.
- Control of Substances Hazardous to Health Regulations (2002)
- Decontamination policy
- Health and Safety at Work act (1974)
- Health and Social Care Act (Hygiene code) 2008. with update in 2010.
- Management of Health and Safety at Work Regulations (1999)
10 References
- Health Service Guidelines (1995) Hospital Laundry Arrangements for Used and Infected Linen, HSG(95) 18 to 21 April 1995.
- Choices Framework for Local Policy and Procedures 1 to 4 version 1.
- Ayliffe G.A.J., Babb J.R., Taylor L.J., (2001), Hospital Acquired Infection, Principles and Prevention. Butterworth Heinemann, third edition, page 168.
- Royal College of Nursing (2006) Guidance on Uniforms and Clothing Worn in the delivery of Patient Care. RCN Wipe it out Campaign.
11 Appendices
11.1 Appendix A Laundry bin system
Ideally patient clothing should not be laundered on the wards unless it is part of a patient’s rehabilitation plan. It should either be taken home by relatives or carers or sent to the main laundry at Tickhill Road Site following the flow chart below.
Note, patients’ clothing must be labelled with their name and the ward or area before sending to the trust laundry so that it can be returned to the individual
An explanation of the laundry bin system is as follows and is also shown in a flow chart diagram:
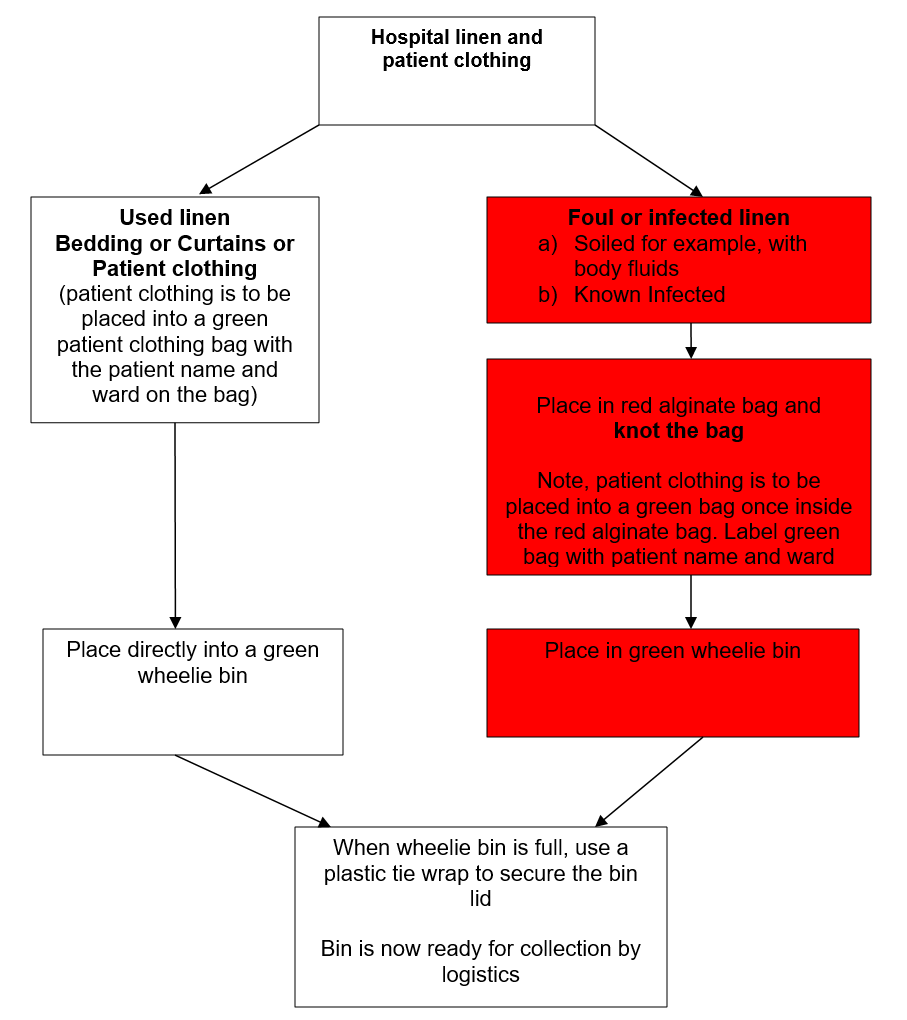
Used hospital linen (bedding and curtains) are to be placed directly into a green wheelie bin. When the wheelie bin is full, it should be secured with a plastic tie wrap which has the wards name on it. Logistics will collect the full wheelie during their scheduled run and take to the laundry for processing. Any patient clothing for laundering on the TRH site must be placed in a green patient clothing bag with the patient name or ward name, and the bag is to be placed in the green wheelie bin.
Foul or infected linen are items which are soiled with bodily fluids that have been used in an area with a known infection. All foul or infected linen is to be placed in a red alginate bag and the bag is to be knotted. The tied red alginate bag is to be placed in the green wheelie bin. When the wheelie bin is full, it should be secured with a plastic tie wrap which has the wards name on it.
Document control
- Version: 10.
- Unique reference number: 64.
- Approved by: Corporate policy approval group.
- Date approved: 6 February 2024.
- Name of originator or author: Head of facilities.
- Name of responsible committee or individual: Executive director of finance and estates.
- Date issued: 9 February 2024.
- Review date: 28 February 2027.
- Target audience: This policy is applicable to all staff and managers of staff who in the course of their work will be involved in the handling, transportation, labelling, washing and processing linen and, where applicable, patients’ clothing.
Page last reviewed: December 06, 2024
Next review due: December 06, 2025
Problem with this page?
Please tell us about any problems you have found with this web page.
Report a problem