Contents
1 Policy summary
This policy applies to all colleagues employed by, or undertaking duties on behalf of, the trust who work within bed-based services.
The policy supports colleagues to provide care in a way which is respectful and maintains privacy and dignity.
Every patient has the right to receive high quality care that is safe, effective and respects their privacy and dignity. This is one of the guiding principles of the NHS constitution and responsibility for these rights does not lie with one individual or group, but with all colleagues at all levels. Providers of NHS-funded care are expected to have a zero-tolerance approach to mixed-sex accommodation, except where it is in the overall best interest of all patients affected.
1.1 Quick guide
1.1.1 Possible breach of policy
Consider whether:
- acceptable justification
- unacceptable justification
- patient choice
- exceptional circumstances
1.1.2 Trans people
- Ensure they are accommodated with the gender they identify with
1.1.3 No bed available
- Follow the flow chart applicable to the inpatient area
1.1.4 Breach of policy
- Report using the IR1 system
2 Introduction
The National Health Service (NHS) Operating Framework issued in 2011, required all providers of NHS funded care to confirm whether they are compliant with the national definition “to eliminate mixed sex accommodation except where it is in the overall best interests of the patient or reflects their patient choice”. This reporting requirement remains in place.
Being with other patients of the same gender is an important component of privacy and dignity. It is a requirement that the trust provides wards and services in single gender bays and has segregated washing and toilet facilities to allow for patients’ dignity.
The Health and Social Care Act (2008) (Regulated Activities) Regulations 2014: Regulation 10 requires providers to ensure that patients are treated with respect and dignity at all times. This includes making sure that patients have privacy when they need and want it, treating them as equals and providing any support they might need to be autonomous, independent, and involved in their community. This regulation is monitored by the Care Quality Commission (CQC) who can take regulatory action if this is breached.
The NHS Constitution for England (2021) states that patient experience is the most important measure of success. Positive patient experience is important and that patients report feeling that their right to privacy, dignity and respect is upheld and actively promoted by colleagues and that they feel they always matter.
The trust is required and committed to deliver same sex accommodation to enhance the privacy and dignity of patients. The trust believes that every patient, regardless of gender identity, has the right to receive high quality care that is safe, effective and respects their dignity and this is one of the guiding principles of the NHS Constitution. There are no exceptions to delivering high standards of privacy and dignity and colleagues should always take the utmost care to respect this.
3 Purpose
This policy is designed to provide:
- direction to provide care and treatment to all patients and carers receiving services from the trust in a way which treats them with respect and maintains their right to privacy and dignity
- a clear definition of privacy and dignity within a care setting
- a clear definition to all in-patient colleagues of same sex accommodation
- in-patient colleagues across the trust with guidance on the safe management of same sex accommodation
- details of the procedure for reporting any breaches in the trust compliance in relation to eliminating mixed sex accommodation
4 Scope
This policy applies to:
- all colleagues working for or on behalf of the trust, including contracted third parties, agency colleagues, locums, students or trainees, secondees, colleagues from partner organisations with approved access, visiting colleagues, researchers, companies providing other services to the trust for example, IT and all volunteers
- any trust healthcare records held, maintained, and managed by third parties under contract to the trust.
For further information about responsibilities, accountabilities and duties of all colleagues, please see appendix A.
5 Definitions
| Term | Definition |
|---|---|
| Same sex wards | Wards with all facilities, including dedicated toilet and washing facilities, occupied solely by either men or women, boys or girls |
| Mixed sex wards | Wards with single bedrooms and same gender toilet and washing facilities (preferably ensuite) |
| Mixed sex wards | Wards with bed bays (multi-bedded rooms) occupied exclusively by either men or women with access to same-gender toilet and washing facilities |
| Female only lounges | In consideration of the fact that due to their illness, the capacity of patients within the mental health and learning disability inpatient services can be impaired which increases their level of vulnerability it is essential that within these areas female only lounges are provided |
| Privacy | Refers to freedom from intrusion and relates to all information and practice that is personal or sensitive in nature to an individual (DOH, 2009). Privacy is a key principle, which underpins human dignity, and remains a basic human right and the reasonable expectation of every person (Human Rights Act,1998)
The seven privacy and dignity benchmarks are:
|
| Dignity
|
To treat someone with dignity is to treat them as being of worth, in a way that is respectful of them as valued individuals, being of equal value and worth irrespective of differences such as age, race, culture, gender, sexual orientation, social background, health or marital status, disability, religion or political conviction.
In care situations, dignity may be promoted or diminished:
Dignity applies equally to those have capacity and to those who lack it (Royal College of Nursing, 2008) |
| Respect | is positive regard shown to a person as a human being as an individual, by others, and demonstrated as courtesy, good communication, taking time and equal access |
| Privacy | In terms of personal space: modesty and privacy in personal care; and confidentiality of treatment and personal information |
| Self esteem, self-worth, identity and a sense of oneself | Promoted by all the elements of dignity but also by ‘all the little things’- a clean and respectable appearance, pleasant environments and by choice and being listened to |
| Autonomy | Including freedom of act and freedom to decide on opportunities to participate, and clear comprehensive information |
| Modesty: | Refers to treatment being given in a manner which avoids unnecessary exposure and minimises anxiety and distress |
5.1 Sex versus gender
Sex and gender are terms that are often used interchangeably but are in fact two different concepts. The UK government (Office of National Statistics, 2019) defines sex as:
- referring to the biological aspects of an individual as determined by their anatomy, which is produced by their chromosomes, hormones and their interactions
- generally male or female
- something that is assigned at birth.
The UK government defines gender as:
- a social construction relating to behaviours and attributes based on labels of masculinity and femininity; gender identity is a personal, internal perception of oneself and so the gender category someone identifies with may not match the sex they were assigned at birth where an individual may see themselves as a man, a woman, as having no gender, or as having a non-binary gender, where people identify as somewhere on a spectrum between man and woman
6 Procedure or implementation
6.1 Good practice guide
In mixed-sex wards, it is good practice to create separate parts of the ward for men and women and designated areas or zones, for the bedrooms and toilet or washing facilities for each gender. There may be times, albeit not ideal, when a corridor or the bedroom area of a ward may be mixed. If this occurs, bedrooms, toilet and bathing facilities should be designated to achieve as much gender separation as possible and care supported by appropriate staffing. Each inpatient area has in place guidance which colleagues are to refer to for full details as to the safe management of instances when male and female patients need to be accommodated on the same bedroom corridor (appendix C, D, E).
Transgender patient care is shown in appendix F.
Men and women should not have to pass through the bedrooms or bed bays of the opposite gender to access their own bedrooms or toilet or washing facilities. Ideally, patients should not pass through mixed, communal areas adjacent to their bedrooms or bed bays to access their washing facilities. The exception is toilet facilities used while in day areas where patients are fully dressed.
Some toilets and bathrooms contain specialist facilities which are fixed (for example, hoists) to make them accessible for disabled users. Such facilities may be designated unisex if they are for use by one person at a time, are lockable from the inside (with external override) a risk assessment has been conducted and where necessary, the patient is escorted by a colleague. The ideal remains to have segregated accessible facilities where this is possible.
6.2 Breaches of policy
Care Quality Commission supporting note mixed sex accommodation (opens in new window).
A breach occurs at the point a patient is admitted to mixed sex accommodation outside the terms of this policy or if a female only lounge in a Mental Health or learning disability facility is not available.
Mixing may be justified (for example, not a breach) if it is in the overall best interest of the patient, or reflects their personal choice.
6.3 Reporting of breaches
All potential breaches of sleeping accommodation must be reported for each patient affected via the trust incident reporting system IR1.
6.4 Acceptable justification physical health (not a breach only)
- In the event of a life-threatening emergency either on admission or due to sudden deterioration in a patient’s condition.
- Where a critically ill patient requires constant one-to-one nursing.
- Where a nurse must be always physically present in the room or bay.
- Where a short period of close patient observation is needed, for example, where there is a high risk of adverse drug reaction.
- On the joint admission of couples or family groups.
6.5 Unacceptable justification (a breach)
- Placing a patient in mixed-sex accommodation for the convenience of medical, nursing, or other colleagues, or from a desire to group patients within a clinical speciality.
- Placing a patient in mixed-sex accommodation because of a shortage of colleagues or poor skill mix.
- Because of restrictions imposed by old estate (for example, old buildings and facilities are not considered an excuse for non-compliance).
- Placing a patient in mixed-sex accommodation because of a shortage of beds.
- Placing a patient in mixed-sex accommodation because of a fluctuation in activity or seasonal pressures.
- Placing a patient in mixed-sex accommodation because of a predictable non-clinical incident, for example, ward closure.
- Placing or leaving a patient in mixed sex accommodation whilst waiting for assessment, treatment, or a clinical decision.
- Placing a patient in mixed sex accommodation for regular but not constant observation.
- Placing a patient in a mixed sex accommodation because of bed availability or shortage of beds.
- If policy is breached due to bed availability a clinical senior discussion has to take place between matrons or nurse directors.
It is not acceptable to mix genders purely based on clinical specialism. For instance, in a stroke unit, it may be acceptable to mix patients immediately following admission (life threatening emergency, and in need of 1-to-1 nursing) but not to maintain mixing throughout their rehabilitation phase, simply on the basis that it is easier for colleagues, or because there are not enough colleagues with the necessary skills.
6.6 Patient choice
There are some instances when sharing accommodation with the opposite gender reflects personal choice and may therefore be justified. In all cases, privacy and dignity should be assured. Group decisions should be reconsidered for each new admission to the group as consent cannot be presumed and, in such circumstances, consideration needs to be given to the patient’s capacity to make a choice.
There are certain situations where it is in the patient’s best interest to receive rapid or specialist treatment, and same–sex accommodation is not the immediate priority. In these cases, privacy and dignity must be protected. The patient should be provided with same–sex accommodation immediately the acceptable justification ceases to apply.
6.7 Acceptable justification (not a breach)
- If an entire patient group has expressed an active preference for sharing and all patients have the capacity to express their preference.
- If individual patients have specifically asked to share and other patients are not adversely affected (for example, children and young people who have expressed an active preference for sharing with people of their own age group, rather than gender)
6.8 Unacceptable justification (a breach)
- “Take it or leave it” for example, if the patient is asked to choose between accepting mixed-sex accommodation, or going elsewhere
- “No win situation” the patient is asked to prioritise same-sex accommodation over another aspect of their care for example, speed of admission, specialist colleagues.
- Custom and practice, for example, routine mixing of young people without establishing preferences.
- If the patient said they did not mind (there should always be a presumption of segregation unless patients specifically ask to share).
- If the patient did not express a preference.
It is important to note that it is always the priority to aim for segregation; the circumstances in which patients choose to share are expected to be in the minority.
6.9 Exceptional circumstances
There will be specific circumstances where mixing is acceptable as an emergency to extreme operational emergencies. This is limited to unpredictable events such as major clinical incidents for example, a multiple road traffic accident or natural disaster and major non-clinical incidents such as fire, or flood requiring immediate evacuation of buildings. The business continuity plans for each of the trust’s individual services or departments will support the ongoing provision of same sex accommodation during these circumstances.
6.10 Maintaining same sex accommodation in the event of an outbreak
The trust’s major incident plan sets out a framework for organisational responses to any kind of major incident affecting patients and colleagues. This alongside the business continuity plans for each of the trust’s individual services and departments will support the ongoing provision of same sex accommodation during any such outbreak.
6.11 Special considerations
6.11.1 Single sex wards
Within the trust there are several single sex wards, but this policy still applies to these in relation to the maintenance of patient’s privacy and dignity, and the right of the patients to be treated with respect.
6.11.2 Transgender patients and Equality Act
For consideration of trans patients and the Equality Act, refer to the patient trans equality policy appendix A (opens in new window) summarises consideration for in-patient stays.
A flow chart of consideration is included in appendix F to support decision-making.
A trans, gender fluid or non-binary person has equal rights to access single gendered accommodation as any other person and therefore should be admitted in accordance with their presenting gender identify. It is good practice to involve the patient, as much as possible, in the admission process. This can help reassure the patient and help colleagues understand what they can do to support the Trans person.
Trans, gender fluid or non-binary persons should be accommodated according to the gender they identify with. This may or may not be related to their current presentation, for example, dress or name and it is important to discuss and clarify with the person when it is appropriate to do so.
6.12 Electro convulsive therapy
Within Rotherham, Doncaster and South Humber NHS Foundation Trust there is one Electroconvulsive therapy (ECT) department based at the Woodlands Older peoples Mental Health Unit at Oakwood Hall Drive Rotherham. This service delivers same sex accommodation, based on the following being in place:
- delivering same sex accommodation within the ECT department
- all patients attend the department wearing their own loose-fitting clothing
- treatment is coordinated, so there is only one patient in the treatment room, and one patient in the recovery room
- patient flow through the department is controlled by the lead clinician to enable all patients to receive their treatment, and recovery with patients of the same sex, this covers any emergency situation where there may need to be more than one patient in recovery
Please see electro convulsive therapy policy for further information.
7 Training implications
There are no specific training needs in relation to this policy, but all trust colleagues must be familiar with its contents.
As a trust policy, all colleagues must be aware of the key points that the policy covers. Colleagues can be made aware through a variety of means such as:
- staff app
- practice development days
- corporate induction days
- half day learning events
- team meetings
- supervision
- practice development days
8 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
8.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
8.1.1 How this will be met
The content of this policy emphasises the need throughout that the patient’s privacy and dignity are respected.
8.2 Mental Capacity Act (2005)
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals’ capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act (2005).
9 Links to any other associated documents
- MCA Mental Capacity Act (2005) policy
- Electro-convulsive therapy (ECT) clinical guidelines policy
- Policy for consent to examination and treatment
- Policy for the provision of access to and use of interpreters
- Safeguarding adults policy
- Critical and major incident plan
- Patient trans equality policy
10 References
- Department of Health (2008b) High Quality Care for All: NHS Next stage Review Final Report (opens in new window).
- Department of Health (2011) The Operating Framework for the NHS in England 2012/2013 (opens in new window).
- Department of Health and Social Care (2021) The NHS Constitution for England (opens in new window).
- Dhejne et al. (2011) Long-term follow up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden (opens in new window).
- Health and Social Care Act 2008 (Regulated Activities) Regulations 2014: Regulation 10. (opens in new window).
- HM Government (1998) Human Rights Act (opens in new window).
- HM Government (2003) Criminal Justice Act (opens in new window).
- HM Government (2004) Gender Recognition Act (opens in new window).
- HM Government (2005) Mental Capacity Act (opens in new window).
- HM Government (2010) Equality Act (opens in new window).
- NHS England and NHS Improvement (2019) Delivering same-sex accommodation. (opens in new window).
- Office for National Statistics (2019) What is the difference between sex and gender? (opens in new window).
- Whittle, et al. (2007) Endangered penalties: Transgender and transsexual people’s experiences of inequality and discrimination (opens in new window).
11 Appendices
11.1 Appendix A Responsibilities, accountabilities and duties
The trust has a duty of care and a duty of confidentiality to ensure that all aspects of healthcare record keeping are properly managed. The trust must adhere to the legislative, statutory, and good practice guidance requirements relating to healthcare records management.
The chief executive has overall accountability and responsibility for healthcare records within the trust. This function is delegated to the executive medical director and the chief nurse who are responsible for driving high quality standards of healthcare record keeping.
The trust’s executive medical director (and trust Caldicott guardian) plays a key role in ensuring that NHS and partner organisations comply with current national guidance and relevant legislation regarding the handling and safeguarding of patient identifiable information. The Caldicott guardian will advise colleagues on matters relating to the management of patient identifiable information, for example where issues such as the public interest conflicts with duties such as maintaining confidentiality.
Care group directors are responsible for the quality of the healthcare records that are generated by all trust colleagues to ensure patient safety and quality service delivery.
Head of information management and business intelligence will advise the trust on how to maintain an efficient and effective patient information system, which complies with all the data collections required within the NHS.
Healthcare professionals must:
- actively promote the patient’s privacy and dignity at all times
- ensure that all patients are cared for in single sex accommodation as defined by this policy
- be aware of their role if acting as a chaperone
- report any breaches of the policy or EMSA to their line manager and on the trust’s incident reporting system (IR1).
11.2 Appendix B Monitoring arrangements
11.2.1 Breaches of eliminating same sex accommodation
- How and who by: Investigation of any IR1 reports which relate to breaches of EMSA. By nurse consultant for safeguarding
- Reported to: Trust performance reports.
- Frequency: By exception.
11.2.1 Compliance with eliminating same sex accommodation
- How and who by: Report. By nurse consultant for safeguarding
- Reported to: Quality committee.
- Frequency: Annually.
11.3 Appendix C Bed management and delivering single sex accommodation on the adult acute mental health wards (Rotherham and Doncaster)
Whilst the adult acute mental health wards are not single sex, they are designed to provide single en-suite bedrooms on corridors which are designated as single sex. However due to demand for inpatient beds there may be times when the ratio of male and female patients is not balanced to the available beds and in these circumstances, colleagues should take the following action:
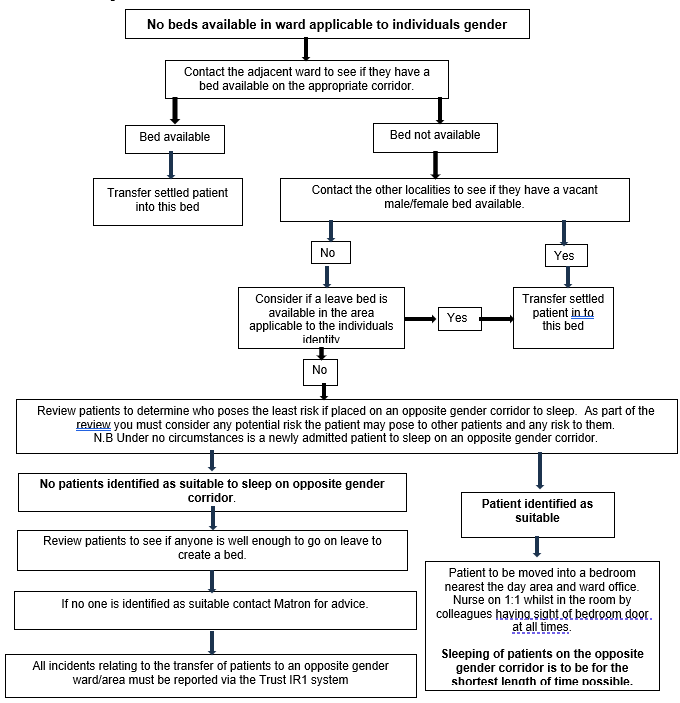
- No beds available in ward applicable to individuals gender.
- Contact the adjacent ward to see if they have a bed available on the appropriate corridor.
11.3.1 Bed available
- Transfer settled patient into this bed.
11.3.1 Bed not available
- Contact the other localities to see if they have a vacant male and female bed available.
11.3.1.1 Other localities have a bed available
- Transfer settled patient into this bed.
11.3.1.2 Other localities do not have a bed available
- Consider if a leave bed is available in the area applicable to the individuals’ identity, if it is transfer settled patient into this bed.
- If not, review patients to determine who poses the least risk if placed on an opposite gender corridor to sleep. As part of the review you must consider any potential risk the patient may pose to other patients and any risk to them. Note under no circumstances is a newly admitted patient to sleep on an opposite gender corridor.
- If patient identified as suitable is to be moved in to a bedroom nearest the day area and ward office. Nurse on 1-to-1 whilst in the room by staff having sight of bedroom door at all times whilst patient is in room. Sleeping of patients on the opposite gender corridor is to be for the shortest length of time possible.
- If no patient identified as suitable to sleep on opposite gender corridor. Review patients to see if anyone is well enough to go on leave to create a bed. If no one is identified as suitable contact modern matron for advice. All incidents relating to the transfer of patients to an opposite gender ward or area need to be reported via the trust IR1 system.
11.4 Appendix D Bed management and delivering single sex accommodation on inpatients ward (North Lincolnshire)
Whilst Laurel ward is not single sex, it is designed to provide single en-suite bedrooms within zones in corridors which are designated as single sex. However due to demand for inpatient beds there may be times when the ratio of male and female patients is not balanced to the available beds and in these circumstances, colleagues should take the following action:
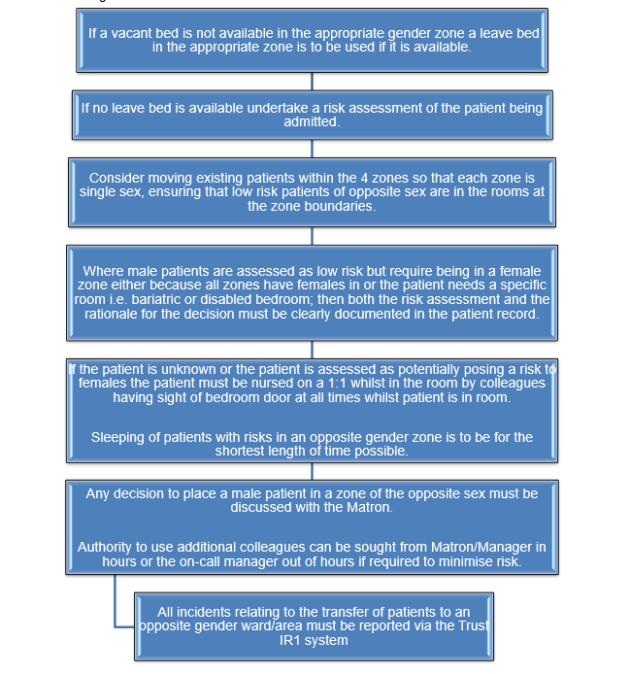
- If a vacant bed is not available in the appropriate gender zone a leave bed in the appropriate zone is to be used if it is available.
- If no leave bed is available undertake a risk assessment of the patient being admitted.
- Consider moving existing patients within the 4 zones so that each zone is single sex, ensuring that low risk patients of opposite sex are in the rooms at the zone boundaries.
- Where male patients are assessed as low risk but require being in a female zone either because all zones have females in or the patient needs a specific room, for example, bariatric or disabled bedroom; then both the risk assessment and the rationale for the decision must be clearly documented in the patient record.
- If the patient is unknown or the patient is assessed as potentially posing a risk to females the patient must be nursed on a 1-to-1 whilst in the room by colleagues having sight of bedroom door at all times whilst patient is in room. Sleeping of patients with risks in an opposite gender zone is to be for the shortest length of time possible.
- Any decision to place a male patient in a zone of the opposite sex must be discussed with the matron. Authority to use additional colleagues can be sought from matron or manager in hours or the on call manager out of hours if required to minimise risk.
- All incidents relating to the transfer of patients to an opposite gender ward or area need to be reported via the trust IR1 system.
11.5 Appendix E Bed management and delivery of single sex accommodation on Hazel, Hawthorn and Magnolia
Hazel, Hawthorn and Magnolia are mixed sex wards with single sex bays and single rooms. When selecting appropriate placement staff need to consider dignity of new patient and others. Document decision-making process in care plan.
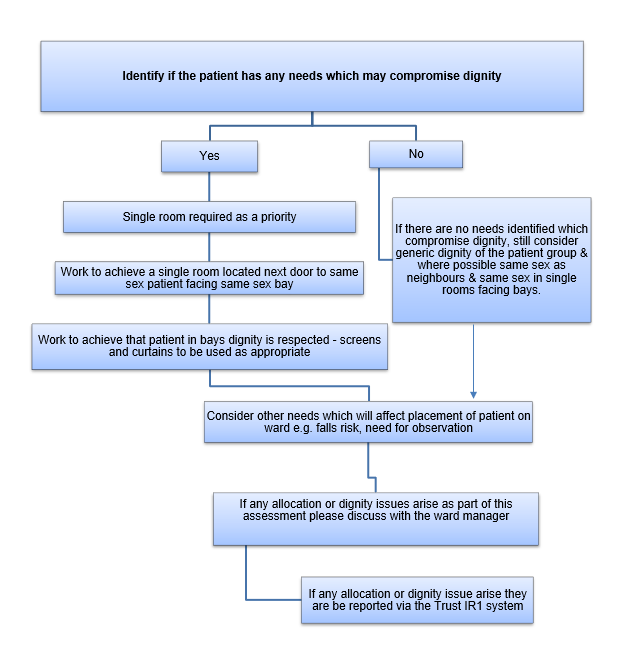
Identify if patient has any needs which may compromise dignity.
11.5.1 If the patient has no needs that compromise dignity
- If there are no needs identified which compromise dignity, still consider generic dignity of the patient group and where possible same sex as neighbours and same sex in single rooms facing bays.
- Consider other needs which will affect placement of patient on ward. For example, fall risk, need for observation.
- If any allocation or dignity issues arise as part of this assessment please discuss with ward manager matron.
- If any allocation or dignity issue arise they are to be reported via the trust IR1 system.
11.5.2 If the patient has needs that compromise dignity
- Single room required as priority.
- Work to achieve a single room located next door to same sex patient and facing same sex bay.
- Work to achieve that patient in bays dignity is respected, screens and curtains to be used as appropriate.
- Consider other needs which will affect placement of patient on ward. For example, fall risk, need for observation.
- If any allocation or dignity issues arise as part of this assessment please discuss with ward manager matron.
- If any allocation or dignity issue arise they are to be reported via the trust IR1 system.
11.6 Appendix F Trans patient admission
11.6.1 Supporting transgender patient admission pathway
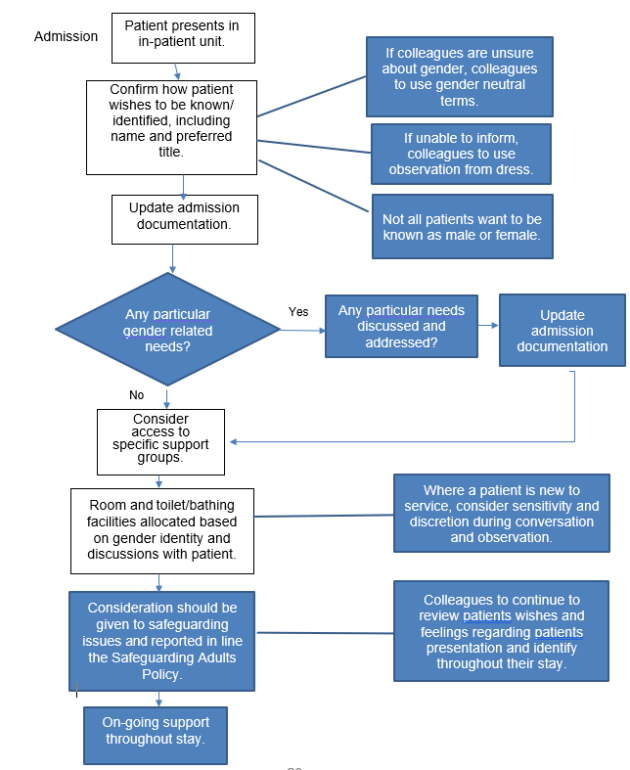
- Patient presents in inpatient unit.
- Confirm how patient wishes to be known or identified, including name and preferred title:
- if colleagues are unsure about gender, colleagues to use gender neutral terms
- if unable to inform colleagues to use observation from dress
- not all patients want to be known as male and female
- Update admission documentation
- Any particular gender related needs?
- If yes, any particular needs discussed and addressed? If available, update admission documentation.
- Consider access to specific support groups.
- Room and toilet or bathing facilities allocated based on gender identity and discussions with patient. Where a patient is new to service, consider sensitivity and discretion during conversation and observation.
- Consideration should be given to safeguarding issues and reported in line the safeguarding adults policy. Colleagues to continue to review patients wishes and feelings regarding patients presentation and identify throughout their stay.
- Ongoing support throughout stay.
11.7 Appendix G Bed management and delivery of single sex accommodation at new beginnings in-patient unit
New Beginnings inpatient unit is a mixed sex ward with twelve single rooms, 8 rooms have en-suite facilities including a toilet and shower and 4 rooms have shared facilities which are allocated to same sex patients, there is also a women’s only lounge. All admissions are planned and have a scheduled length of admission. All patient episodes are approximately 14 days. There may be times when the ratio of male and female patients is not balanced, but this is managed. When selecting appropriate placement of patients, colleagues need to consider the dignity of new patient and others. Colleagues should document their decision-making process in the patients care plan in the electronic patient record.

Identify if patient has any needs which may compromise dignity.
11.7.1 If the patient has no needs that compromise dignity
- If there are no needs identified which compromise dignity, still consider generic dignity of the patient group and where possible same sex as neighbours, same sex where a shared toilet is between two rooms.
11.7.2 If the patient has needs that compromise dignity
- Work to achieve an en-suite room located next door to same sex patient ideally.
- Consider other needs which will affect placement of patient on ward, for example, falls risk, need for observation.
- If any allocation or dignity issues arise as part of this assessment please discuss with the clinical team leader and senior nurse.
- If any allocation or dignity issue arise they are to be reported via the trust IR1 system.
Document control
- Version: 5.
- Unique reference number: 339.
- Approved by: Clinical policies review and approval group.
- Date approved: 18 September 2024.
- Name of originator or author: Deputy director of nursing.
- Name of responsible individual: Chief nurse.
- Date issued: 26 September 2024.
- Review date: 30 September 2027.
- Target audience: All staff working on in patient areas.
Page last reviewed: January 17, 2025
Next review due: January 17, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.