Content
- Introduction
- Purpose
- Scope
- Responsibilities, accountabilities and duties
- Procedure and implementation
- Training implications
- Monitoring arrangements
- Equality impact assessment screening
- Links to associated policies or documents
- References to further reading
- Appendices
1 Introduction
1.1 Continence care
Incontinence is not a disease but a symptom of an underlying condition. Through informed assessment and investigation by a suitably trained professional, individuals suffering from bladder or bowel dysfunction may have symptoms resolved, improved or managed in the most appropriate way, without the primary focus placed on the supply of continence products. The importance of the assessment cannot be overestimated, as treatment for continence is dependent on the cause(s) (Button et al., 1999).
1.2 Urinary catheterisation
Urinary catheterisation is a common procedure both in acute and community settings. Catheterisation is not without risk, urinary tract infections (UTI’s) are the largest single group of Healthcare Associated Infections (HCAI) and the presence of a urinary catheter and the duration of its insertion are contributory factors to the development of urinary tract infection. (Emmerson, 1996). Therefore, urinary catheters should only be used when there is no suitable alternative, and even then kept in place for as short a time as possible, (NICE, 2012).
1.3 Referral pathway into the specialist continence service (SCS)
The registered healthcare professional remains accountable for the initial assessment of continence and instigation of first line treatment, such as fluid and basic constipation advice, following guidance from the trigger questions (see appendix A). Referral to the SCS should then be made if symptoms persist.
The SCS accepts referrals for the following:
- patients who require a comprehensive bladder and bowel assessment and treatment
- for assessment for trans anal irrigation
- trial without catheters
- intermittent self catheterisation and intermittent self dilatation
- non-housebound catheter patients for catheter clinic
- complex bladder and bowel patients
- for the long term management of catheter products, excluding housebound patients with long term Indwelling catheters
Patients aged over 18, registered with a Doncaster GP may be referred by the following:
- community nursing services
- primary care
- secondary care
- social care providers
- care homes (with or without nursing)
- other Healthcare providers
Referrals to the SCS can be made by electronic referral SystmOne or via email to single point of access (SPA) following completion of a referral form (appendix B). All referrals will be triaged by an appropriate member of the SCS team. The patient will be assessed for eligibility and acuity based on the following tiered criteria:
- urgent, assessments for patients not already on the SCS caseload, presenting with sudden incontinence
- non-urgent, assessment or follow-up for patients on the SCS caseload with a recurring issue or mild exacerbation
- planned, scheduling of planned activity, for example, trial without catheter (TWOCs) to support patients discharged in to the community
Patients, or their carer and advocate, should be asked to complete a symptom diary for the appropriate period of time, with an appointment being offered within a maximum of 15 working days from receipt of referral.
1.4 Contact information
Specialist continence advice can be obtained from the trust specialist continence service on 01302 566999.
2 Purpose
The purpose of the manual and the linked procedures is to provide clear, concise guidance on continence and urinary catheter care for all staff whether in a direct or indirect patient care role, regardless of the care environment. It is acknowledged that some staff work in premises over which they have little or no control (for example, patient’s own homes), therefore in some instances staff will have to use their own judgement in the interpretation of certain procedures.
The content of the manual and linked procedures is based on sound specialist continence principles and national guidance.
3 Scope
This manual applies to all clinical staff working in the Doncaster care group of RDaSH who deliver or provide continence or catheter care to adult patients over the age of 18. It is recognised that primary care practitioners are also part of the organisation and as such this manual is offered for use by them to adapt to their own practices and organisations as appropriate. The author of the manual is available to offer help and support to primary care practitioners who wish to use and implement this manual. As part of good employment practice,
agency workers are also required to abide by the RDaSH policies and procedures, as appropriate, to ensure their health, safety and welfare whilst undertaking work for RDaSH.
Adherence to the procedures within this manual is the responsibility of all trust staff, including agency, locum and bank staff. For staff working in Rotherham and Scunthorpe, they will need to refer to local guidelines.
4 Responsibilities, accountabilities and duties
4.1 Chief executive
The chief executive is responsible for ensuring the trust employs a comprehensive strategy to support the management of risk, including clinical risks associated with patient care across the organisation.
4.2 Board of directors
The board of directors is responsible for having policies and procedures in place to support best practice, effective management, service delivery, management of associated risks and meet national and local legislation.
4.3 Care group directors
Care group directors are responsible for the implementation of the policy within their specific areas.
4.4 Specialist continence nurse
The role of the specialist continence nurse includes:
- providing expert professional advice on bladder and bowel care, delegating responsibility to trust staff as appropriate
- providing education on bladder and bowel care to other professionals, multi-disciplinary groups, patients and carers
- assess, plan, deliver and evaluate person centred continence care to patients, in a variety of different care settings, including, patients own home, clinic and care homes
- managing the complex patients referred to the service
- undertake continence and catheter audits in care homes, reporting outcome to Doncaster clinical commissioning group (CCG)
- contributing to serious incidents (SIs) reports as required
4.5 Clinical team leaders or ward managers
Clinical team leaders or ward managers’ duties and responsibilities for areas under their control ensure that staff:
- can demonstrate compliance with the manual and the continence formulary
- are given protected time to attend the relevant continence and catheter study days
4.6 Clinical staff
All staff who are involved with the care of a patient within the inpatient services and community must comply with this manual and procedures.
It is the responsibility of each individual member of staff to adhere to the requirements set out within this policy.
4.7 Continence link champions
Duties of the continence link champions include:
- acting as a resource within their working environment, for patients, staff and visitors
- acting as role models, encouraging good continence care at all times
- liaising closely with the specialist continence service
5 Procedure and implementation
These will be listed here on the webpage as hyperlinks to each procedure document along with appendices, references and so on.
- Autonomic Dysreflexia safe management of bladder and bowel care procedure
- Basic catheter care
- Portable bladder scanner use procedure (BVI 3000 or CUBEscan 700)
- Bladder washouts
- Bowel care procedures (in development)
- Catheter maintenance procedure
- Catheter trouble shooting
- Continence products home delivery procedure
- Continence assessment, treatments and provision of pads (in development)
- Female catheterisation and removal procedure
- Intermittent catheterisation procedure
- Male catheterisation and removal procedure
- Managing constipation (in development)
- Trans anal irrigation (in development)
- Trial without catheter procedure
- Urinary catheterisation aftercare procedure
6 Training implication
6.1 Continence care day
- Staffing groups requiring training: District nurses, qualified care home staff, qualified staff TRH.
- How often should this be undertaken: On employment every 3 years.
- Length of training: 9:30am to 4:30pm.
- Delivery method: Presentation.
- Training delivered by whom: SCS team.
- Where are the records attendance held: Electronic staff record system (ESR).
6.2 Continence awareness day
- Staffing groups requiring training: Healthcare assistants, care home care assistance, home carers (DMBC, Age Concern and other private agencies).
- How often should this be undertaken: On employment every 3 years.
- Length of training: 9:30am to 4:30pm.
- Delivery method: Presentation.
- Training delivered by whom: SCS team.
- Where are the records attendance held: Electronic staff record system (ESR).
6.3 Bowel care day
- Staffing groups requiring training: District nurses, qualified care home staff, qualified staff TRH.
- How often should this be undertaken: On employment every 3 years.
- Length of training: 9:30am to 4:30pm.
- Delivery method: Presentation.
- Training delivered by whom: SCS team.
- Where are the records attendance held: Electronic staff record system (ESR).
6.4 Catheter study day
- Staffing groups requiring training: District nurses, qualified care home staff, qualified staff TRH.
- How often should this be undertaken: On employment every 3 years.
- Length of training: 9:30am to 4:30pm.
- Delivery method: Presentation.
- Training delivered by whom: SCS team.
- Where are the records attendance held: Electronic staff record system (ESR).
6.5 Female re-catheterisation study day
- Staffing groups requiring training: Band 3 healthcare.
- How often should this be undertaken: On employment every 3 years.
- Length of training: 9:30am to 4:30pm.
- Delivery method: Presentation.
- Training delivered by whom: SCS team.
- Where are the records attendance held: Electronic staff record system (ESR).
7 Monitoring arrangements
7.1 Training compliance and following up on those who fail to attend
- How: Follow up in writing with relevant trainers and managers.
- Who by: Continence sister.
- Reported to: Community practice educators and managers.
- Frequency: Following every study day.
7.2 Any patient feedback, complaints or your opinion counts which relate to non-compliance with the standards in this policy
- How: Investigation feedback and review.
- Who by: Matrons and managers.
- Reported to: Care group leadership and quality groups.
- Frequency: Ongoing or as the need arises.
8 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
8.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
Consequently, the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity, and respect, (when appropriate this should also include how same sex accommodation is provided).
8.1.1 Indicate how this will be met
Privacy, dignity and respect of the patient will be considered at all times. Sensitivity to the patient’s needs will also be addressed.
8.2 Mental capacity act
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individual’s capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all colleagues working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason, all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected, and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 Indicate how this will be achieved
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act 2005 (section 1). No issues have been identified.
9 Links to any associated documents
- Aseptic non touch technique procedure
- Blood and body fluid spillage procedure
- Chaperoning policy
- Hand hygiene procedure
- Personal protective equipment procedure
- Waste policy
10 References
- Button, D. Roe, B. Webb, C. Frith, T. Colin-Thorne, D. Gardner, L. (1999), Continence Promotion and Management by the Primary Health Care Team. Consensus Guidelines. London, Whurr.
- Department of Health (2000) Good Practice in Continence Services. London, HMSO.
- Department of Health (2001a) National Service Framework for Older People. London, HMSO.
- Emmerson, AM, Enstone, JE, Griffin, M, et al. (1996) The Second National Prevalence Survey of Infection in Hospitals.
- Department of Health (2001b) Medicines and Older People. Implementing medicines related aspects of the NSF for Older People. London, Department of Health.
- National Institute of Clinical Excellence, Infection Control: Preventing Healthcare Associated Infection in primary and community care (2012).
- National Institute of Clinical Excellence, Urinary Incontinence. The Management of Urinary Incontinence In Women. (2015).
- National Institute of Clinical Excellence, Lower Urinary Tract Symptoms in Men (2 National Institute of Clinical Excellence, Faecal Incontinence. The Management of Faecal In continence in Adults (2007).
- National Institute of Clinical Excellence, Guidance on the Management of Irritable Bowel Syndrome in Adults (2015).
- National Institute of Clinical Excellence, Nocturnal enuresis. The Management of Nocturnal enuresis in Children and Young Adults (2010).
- NICE (2012) Infection Control: Preventing Healthcare Associated Infection in Primary and Secondary Care. National Institute of Clinical Excellence, Manchester.
- NHS England, Excellence in Continence Care Framework (2018) Nursing and Midwifery Council (updated 2018) The Code RCN, Catheter Care, RCN Guidance for Health Care Professionals (2019).
11 Appendices
11.1 Appendix A Trigger questions around bladder and bowel symptoms
- Is there any evidence that the patient may have a problem with their bladder or bowels?
- Is there an odour in the house?
- Are there any pads on show in the house?
If yes, ask the patient if they are having any problems with their “water works” or bowels.
- Does it sting or burn when you pass water?
- Is there blood in your water?
| Possible causes | Guidance |
|---|---|
| Infection | Urinalysis and, or MSU. Antibiotic treatment if advocated for clinic signs of infection. If repeated infection requires further investigation |
- Do you leak when you cough, laugh, bend, or lift a heavy object?
| Possible causes | Guidance |
|---|---|
| Stress incontinence due too poor pelvic floor tone | Refer to the Continence Health Advisory Service |
- Do you have an urgent need to use the toilet?
- Do you need to use the toilet frequently?
- Do you ever leak before you reach the toilet?
| Possible causes | Guidance |
|---|---|
| Unstable bladder due to medical condition, for example, MS, CVA, Post Prostatectomy. Poor fluid intake or type of fluids, infection | Bladder retraining. Advice on fluids. Refer to the GP for anticholinergic or antibiotic therapy. If no improvement in 3 months refer to continence health advisory service |
- Do you only pass small amounts of water at a time?
- Does your bladder still feel full after passing water?
- Do you ever have to wait or strain to pass water?
- Is your flow weak?
- Do you have frequent water infections?
- Do you dribble continuously, or after passing water?
| Possible causes | Guidance |
|---|---|
| Incomplete emptying due to enlarge prostate, Stricture, faecal Impaction, neurogenic bladder or Spinal Injuries | Bladder scan (refer to bladder scan flow chart) aids and appliances. Clear impaction. Bladder stimulation, ISC, Refer to continence, Take U and E’s if residual volume greater than 200mls |
- Have sudden wetness without warning?
- Are you ever unaware that you have been incontinent?
| Possible causes | Guidance |
|---|---|
| Passive incontinence due to mental impairment, dementia or confusion | Habit retraining. Aids and appliances. Adapt the environment. Prompting, toilet programme |
- Do you wet the bed?
| Possible causes | Guidance |
|---|---|
| Nocturnal enuresis due to vasopressin deficiency. Over active bladder | Review fluid intake. Review of caffeine intake. Desmopressin, bladder retraining, ISC, anticholinergic community only-referral to laundry services |
- Do you have problems with mobility resulting in incontinence?
- Do you have problems with dexterity resulting in incontinence?
- Do Your present facilities cause or contribute to your incontinence?
- Do you need to be reminded to go to the toilet to prevent incontinence?
| Possible causes | Guidance |
|---|---|
| Functional incontinence due to underlying clinical or environmental problems | Adapt the environment or clothing. Prompting toileting. Refer to Occupational therapist and physiotherapist |
- Do you suffer constipation?
| Possible causes | Guidance |
|---|---|
| High fibre intake, low fluid intake, medication check fluid intake, review fibre intake, review medication | Speak with GP regarding soft laxative. Complete stool chart. No changes in 4 weeks refer to continence health advisory service |
- Do you suffer from loose stools?
| Possible causes | Guidance |
|---|---|
| Infection, constipation, over use of laxatives, query bowel disorders, for example, IBS, diverticular disease etc. | Send stool sample. Review medication, Query overflow. Fibre intake. Stool chart. Refer to continence health advisory service |
11.2 Appendix B Continence health advisory service referral form
11.3 Appendix C Flow chart for bladder scanning
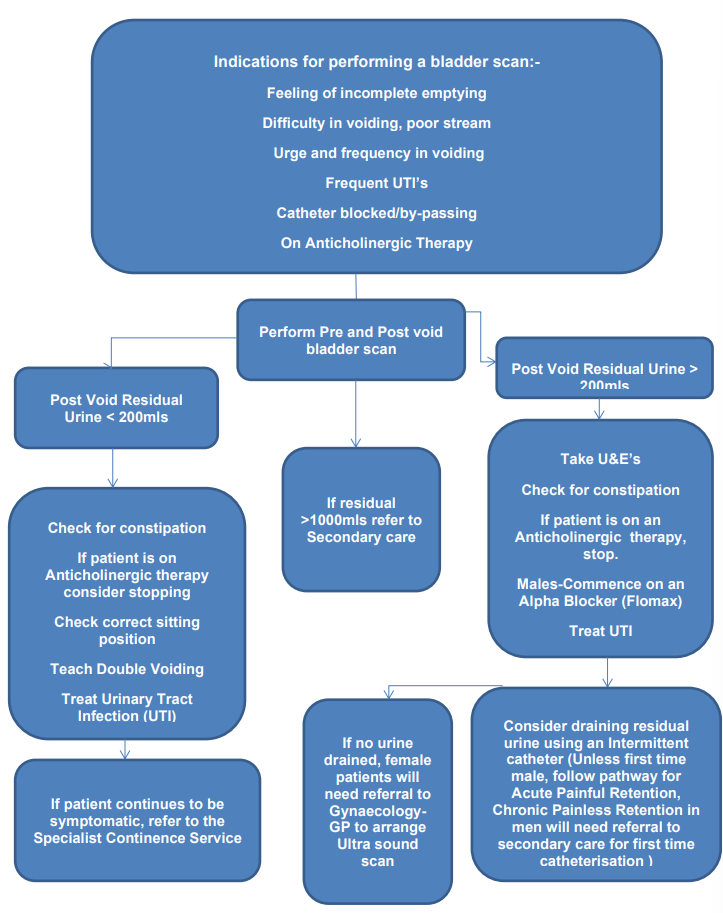
- Indications for performing a bladder scan:
- feeling of incomplete emptying
- difficulty in voiding, poor stream
- urge and frequency in voiding
- frequent UTI’s
- catheter blocked or by-passing
- on anticholinergic therapy
- Perform pre-void bladder scan and post-void bladder scan.
11.3.1 Post void residual urine less than 200mls
- Check for constipation.
- If patient is on anticholinergic therapy consider stopping. Check correct sitting position. Teach double voiding. Treat urinary tract infection (UTI).
- If patient continues to be symptomatic, refer to the specialist continence service.
11.3.2 Residual greater than 1000mls
- Refer to secondary care.
11.3.3 Post void residual urine less than 200mls
- Take U and E’s. Check for constipation. If patient is on an anticholinergic therapy, stop. Males-Commence on an alpha blocker (Flomax). Treat UTI
- Consider draining residual urine using an intermittent catheter (unless first time male, follow pathway for acute painful retention, chronic painless retention in men will need referral to secondary care for first time catheterisation)
- If no urine drained, female patients will need referral to gynaecology GP to arrange ultra sound scan
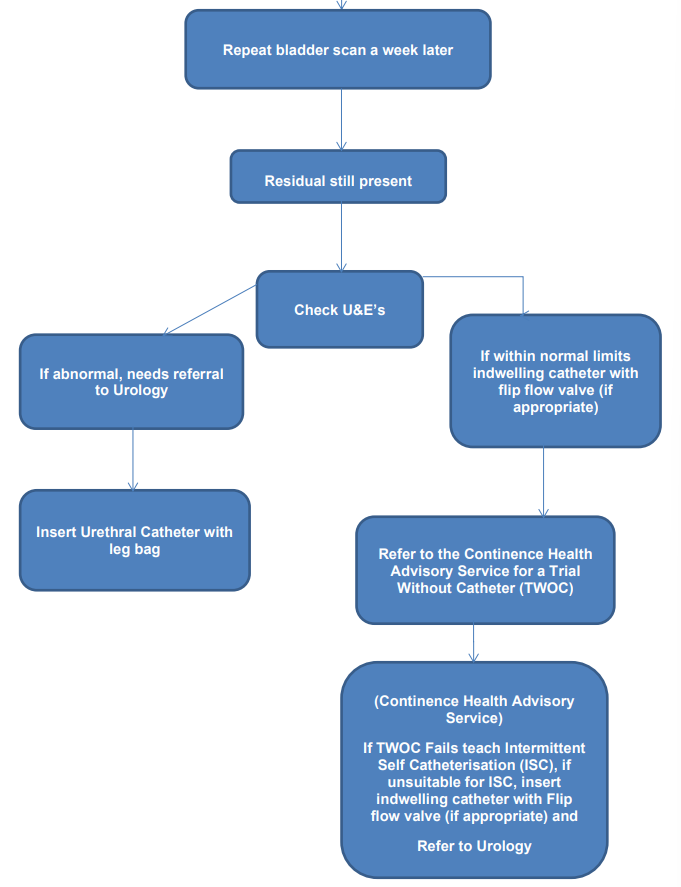
- Repeat bladder scan a week later.
- Residual still present.
- Check U and E’s
11.3.3.1 If abnormal
- Needs referral to urology.
- Insert urethral catheter with leg bag.
11.3.3.2 If within normal limits
- If within normal limits indwelling catheter with flip flow valve (if appropriate).
- Refer to the continence health advisory service for a trial without catheter (TWOC).
- Continence health advisory service, if TWOC fails teach Intermittent self catheterisation (ISC), if unsuitable for ISC, insert indwelling catheter with flip flow valve (if appropriate) and refer to urology.
11.4 Appendix D Trial without catheter procedure
11.4.1 On referral
- Phone the patient to introduce the specialist continence service and assess their understanding of a trial without catheter.
- If a urinary tract infection is present and the patient is on antibiotics, ensure treatment is successful before arranging the TWOC.
- If patient has been discharged from hospital, check to see if patient is known to the Planned Care team for basic catheter care. If not, arrange for a home visit by a continence nurse the following day to discuss basic catheter care, give a catheter passport if this has not been sent home with the patient, to order appropriate catheter equipment and to commence pre TWOC assessment.
- Ask if the patient is using a catheter valve or a leg bag.
- Check patient is not constipated, if the patient is constipated, give advice and follow up within 7 days.
- Add patient to the triage waiting list and explain that a nurse will be in touch as soon as possible to arrange an appointment.
- Provide single point of access (SPA) number for unplanned care team and specialist continence service for support prior to TWOC first time male catheterisation for acute retention referral The trial without catheter needs to be performed within 7 working days. Provisionally book the patient in and add to the triage TWOC waiting list as a priority and notify the triage TWOC nurse. If the patient is not on an alpha blocker, for example, tamsulosin 400mcg at night, inform the patient that the continence sister will be writing to the GP for a prescription to be commenced 48 hours before the TWOC. Advise the patient that they will need to contact their GP practice in 2 working days to follow up on the prescription request.
11.4.2 TWOC triage process
- Check urea and electrolytes (U and E’s) for most recent results. If no recent U and E results available arrange a blood test for U and E’s. If U and E results deranged seek advice from urology. First time male catheterisation, deranged U and E’s repeat in one week and delay TWOC. If U and E’s are within acceptable range, TWOC should be performed within 7 working days. Referrals from accident and emergency (A and E) via urology, TWOC’s should be performed within 14 working days.
- If patient has been catheterised in A and E and no referral has been received from urology, confirm with urology that the patient is safe for a community TWOC to take place. If unable to discuss on the phone schedule a home visit to explain the procedure and complete a trial without catheter pre assessment.
- Contact the patient and discuss the TWOC process and obtain verbal consent.
- Discuss potential risks, and if TWOC is unsuccessful the potential for re-catheterisation.
- If patient has a catheter valve, explain to the patient that on the morning of the TWOC they will need to empty their catheter valve at 6am and then to refrain from emptying it until the nurse visits at 8am to 8:30am. The nurse will then remove that catheter and ask the patient to pass urine.
- If no catheter valve fitted, and U and E’s are within acceptable range, arrange a home visit for a pre-TWOC assessment and assessment for a catheter valve.
- Male patients. If the patient is not on an alpha blocker, for example, tamsulosin 400mcg at night, inform the patient that we will be writing to the GP for a prescription to be commenced 48 hours before the TWOC. Advise the patient will need to contact the GP practice in 2 working days to follow up on the prescription request.
- Check catheter specimen of urine (CSU) results if appropriate.
- Arrange antibiotics with GP if necessary and delay TWOC.
- Check patient is not constipated (will need to delay TWOC if constipated for more than 3 days) if the patient is constipated, give advice and follow up within 7 days.
- Explain to male patients that if the TWOC is successful they will be offered an appointment at 2 weeks in the lower urinary tract clinic for a further review and assessment, this will include assessment of prostate.
11.4.3 Pre TWOC assessment and first visit
- Assess suitability for a catheter valve if required. If the patient has the dexterity and the mental capacity to use a catheter valve, change the catheter bag to a catheter valve.
- Complete a falls assessment if required.
- Consider toilet access for day of the TWOC, is a urinal required?
- Consider HOUDINI assessment for suitability of a catheter.
- Check medication to ensure that those on diuretics are aware of the need to take medication on the morning of the TWOC.
- Check patient is not constipated (will need to delay TWOC if constipated for more than 3 days) if the patient is constipated, give advice and follow up within 7 days.
- Discussed trial without catheter process and obtain verbal consent from the patient.
- Advise patient that they may need to purchase some small pads for during the day of the TWOC.
- Discuss basic catheter care and order appropriate equipment.
- Assess to see if the patient will require a full continence assessment if the TWOC is successful.
11.4.4 Morning of the TWOC between 8am to 8:30am
- Visit patient as planned.
- Assess patient, explain procedure, discuss potential risks and ensure the patient has the contact information for SPA should they have any problems or concerns during the procedure.
- Discuss symptom diary and explain the importance of measuring and recording fluid intake or output during the day. Provide disposable measuring jug if required.
- Only remove catheter if no clinical signs or symptoms of infection, for example, pain or fever and that the patient has given verbal consent to have the catheter removed.
- Explain to the patient that the first void may sting and they may notice a small amount of blood in their urine, this is due to the trauma from removing the catheter.
- Ensure spare equipment is available to facilitate re-catheterisation if required.
- If patient has a catheter valve, ask patient when they last emptied the catheter.
- Remove the catheter using aseptic non touch technique and document in catheter IPOC within SystmOne.
- If the patient has a catheter valve, ask the patient to void straight after removal, and perform immediate post void bladder scan.
- Explain signs and symptoms of urinary retention and ensure the patient has SPA number.
- Instruct the patient to drink one 200mls cup or glass of recommended fluid each hour and to complete Fluid input and output chart.
11.4.5 1pm (5 hours after TWOC)
- Visit the patient as planned, check:
- patient has no discomfort
- has passed urine since catheter was removed
- check fluid input and output chart to ensure patient has been drinking the recommended amounts
- Perform bladder scan.
- If no concerns revisit at 3pm.
If concerns follow process 7 and 8 If at any time the patient becomes uncomfortable and is unable to void consider teaching intermittent self-catheterisation (ISC) or consider an indwelling catheter if ISC is not appropriate 7.
11.4.6 3pm
- Visit the patient as planned, check patient has no discomfort and has passed urine since catheter was removed, check fluid input and output chart to ensure patient has been drinking the recommended amounts.
- Perform bladder scan.
If patient passes urine in good amounts (greater than 50mls) and bladder has Amount Volume TWOC Less than 100mls TWOC successful advise patient on signs of retention and when to seek medical advice. Male patients, advise that they will receive a follow-up appointment in 2 weeks at the lower urinary tract clinic for men if they are not housebound. A letter to their GP will be sent asking for a prostate examination to be performed. Housebound male patients will be followed up at 2 weeks at home Female patients will be followed up at 6 weeks add to the successful TWOC list for review Between 100 to 300mls If patient is asymptomatic of urinary retention, for example, has no pain or discomfort and, or has had a poor fluid intake during the TWOC procedure, arrange a follow-up bladder scan the next day. Discuss with band 6 for advice if required More than 300mls Consider teaching intermittent ISC. If inappropriate, re-catheterise with an indwelling catheter. Consider using a flip flow valve if appropriate. Add to the unsuccessful TWOC list for review - Document actions within the catheter IPOC on SystmOne
11.4.7 Approximately 4pm
Whatever the outcome:
- Inform planned care of outcome if patient is known to them for catheter care.
- Ensure equipment available to facilitate re-catheterisation.
- Arrange a follow-up bladder scan the following day if indicated above.
- Add patient to the appropriate waiting list, for example, successful TWOC or unsuccessful TWOC.
11.4.8 Successful TWOC
- Female patients will be followed up at 6 weeks in either clinic or at home.
- Arrange a full continence assessment if indicated.
- All male patients including the first time male catheterisation pathway management of acute painful retention in men (MAPRIM) will be followed up in the lower urinary tract (LUTS) clinic in 2 weeks, prostate examination to be performed prior to clinic appointment.
11.4.9 Unsuccessful TWOC
- If TWOC is unsuccessful, TWOC to be repeated in 2 weeks.
- If second TWOC fails, the triage TWOC nurse will consider referral to be made to urology.
11.5 Appendix E Trial without catheter procedure hospital wards
11.5.1 Protocol for community hospital wards performing a trial without catheter (TWOC)
Prior to discharge a patient with an indwelling urethral catheter should have TWOC preformed.
Results of the TWOC should be documented on the discharge form. If unsuccessful, results should be documented within the patient’s catheter passport and the catheter IPOC on SystmOne as well.
11.5.2 Pre TWOC assessment
- Consider Houdini assessment for suitability for an indwelling catheter.
- Check urea and electrolytes (U and E’s) for most recent results. If no recent U and E results available arrange a blood test for U and E’s. If U and E results deranged seek advice from urology.
- If no catheter valve fitted, and U and E’s are within acceptable range, assess suitability for a catheter valve. If the patient has the dexterity and the mental capacity to use a catheter valve, change the catheter bag to a catheter valve.
- Male patients, if the patient is not on an alpha blocker, for example, tamsulosin 400mcg at night, inform the patient that we will be writing to the GP for a prescription to be commenced 48 hours before the TWOC.
- Check catheter specimen of urine (CSU) results if appropriate.
- Arrange antibiotics with doctor if necessary and delay TWOC.
- Check patient is not constipated (will need to delay TWOC if constipated for more than 3 days) if the patient is constipated, give advice and follow up 7 days.
- Discuss TWOC process and obtain verbal consent from the patient.
11.5.3 Morning of the TWOC between 8am to 8:30am
- Assess patient, explain procedure and discuss potential risks.
- Discussed symptom diary and explain the importance of measuring and recording fluid intake or output during the day.
- Only remove catheter if no clinical signs or symptoms of infection, for example, pain or fever and that the patient has given verbal consent to have the catheter removed.
- Explain to the patient that the first void may sting and they may notice a small amount of blood in their urine, this is due to the trauma from removing the catheter.
- If patient has a catheter valve, ask patient when they last emptied the catheter.
- Remove the catheter using aseptic non touch technique and document in catheter care record.
- If the patient has a catheter valve, ask the patient to void straight after removal, and perform immediate post void bladder scan.
- Instruct the patient to drink one 200mls cup or glass of recommended fluid each hour. Complete Fluid input and output chart 3.
11.5.4 Midnight (4 hours after TWOC)
- Check patient has no discomfort and has passed urine since catheter was removed, check fluid input and output chart to ensure patient has been drinking the recommended amounts.
- Perform bladder scan.
- If no concerns rescan at 2pm.
- If concerns follow process 7 and 8 If at any time the patient becomes uncomfortable and is unable to void consider teaching intermittent self-catheterisation (ISC) or consider an indwelling catheter if ISC is not appropriate.
11.5.5 2pm (6 hours after TWOC)
- Check patient has no discomfort and has passed urine since catheter was removed, check fluid input and output chart to ensure patient has been drinking the recommended amounts.
- Perform bladder scan.
- If no concerns rescan at 2pm.
- If concerns follow process 5 and 6.
If at any time the patient becomes uncomfortable and is unable to void consider teaching intermittent self-catheterisation (ISC) or consider an indwelling catheter if ISC is not appropriate.
11.5.6 4pm (8 hours after TWOC)
- Check patient has no discomfort and has passed urine since catheter was removed, check fluid input and output chart to ensure patient has been drinking the recommended amounts.
- Perform bladder scan.
| Amount | Volume | TWOC |
|---|---|---|
| Less than | 100mls | TWOC successful advise patient on signs of retention and when to seek medical advice |
| Between | 100 to 300mls | If patient is asymptomatic of urinary retention, for example, has no pain or discomfort and, or has had a poor fluid intake during the TWOC procedure, arrange a follow-up bladder scan the next day |
| More than | 300mls | Consider teaching intermittent ISC. If inappropriate, re-catheterise with an indwelling catheter. Consider using a flip flow valve if appropriate |
- Document outcome within the catheter IPOC on SystmOne.
11.5.7 On Discharge
- Ensure results of the TWOC are clearly documented on the discharge form and within the catheter IPOC on SystmOne including reason for catheterisation.
- If unsuccessful TWOC ensure a catheter passport is completed and given to the patient. A referral to the specialist continence service should be made for a follow-up and a second TWOC.
11.6 Appendix F Managing blocked catheters flow chart
11.6.1 How to establish a catheter maintenance regime and how to manage blocked catheters
- Catheter blocks first time.
- Bladder scan to establish degree of retention.
- Change catheter, document within the catheter IPOC if any encrustation, blood, mucus or debris is evident.
- Catheter block second time, document within the catheter IPOC if any encrustation, blood, mucus or debris is evident.
- Catheter block third time, document within the catheter IPOC if any encrustation, blood, mucus or debris is evident.
- Once a pattern has been established, the use of an appropriate catheter maintenance solution and planned catheter change can be adopted. The effectiveness of the catheter maintenance solution may then be assessed, and the regime altered as necessary (should catheter maintenance be required more than once per week, the use of a bladder infusion kit (BIK) must be used to maintain the closed drainage system PIP or order code MC1/701. If no latex allergies, you may need to consider swapping to a short term catheter.
Catheter maintenance in end-of-life patients:
- if able to determine the cause of a blocked catheter, use the appropriate catheter maintenance solution, Suby-G for encrustation and PHMB for debris or mucus
- if unable to determine cause of the catheter blockage, to administer PHMB twice per week and review (catheter maintenance solution can be administered up to twice per day if required)
If performing catheter maintenance more than once per week, use a Linc medical, bladder infusion Kit (BIK).
If Suby-G is being used daily, please consider changing to the Solutio-R catheter maintenance and reduce the frequency of instillation.
11.6.2 Suby G
Treatment for encrustation, recommended for patients that are identified as a “blocker” due to encrustation. If irritation is experienced, treatment should be halted.
11.6.3 Solutio R
Recommended prior to catheter change and also for persistent “blockers”. Can be effective in clearing a catheter which is completely blocked by encrustation. Prior to catheter removal it will dissolve crystals formed in and around the catheter tip making removal less traumatic, note, Suby G should always be considered first before using the stronger solution of Solutio R.
11.6.4 Normal saline
Recommended to flush out debris and mucus, not suitable for encrustation.
11.6.5 Normal saline with PHMB
Recommended to flush out debris and mucus, not suitable for encrustation. Provides bacterial decolonisation of the catheter
11.7 Appendix G How to administer catheter maintenance solution
| Action | Rationale |
|---|---|
| Explain reasons for procedure and gain consent from patient to undertake procedure | To ensure that patient is able to give informed consent |
| Ensure appropriate solution is prescribed and package is in date | To ensure patient safety |
| Ensure solution is at room temperature | To promote comfort |
| Ensure that patient is positioned comfortably, usually in a supine or sitting position in a private room | To ensure privacy or dignity is maintained |
| Decontaminate hands using alcohol hand gel or liquid soap and water or for community settings soapy hand wipes can be used followed by alcohol hand gel. Note, if in patients own home and hands are decontaminated with soap and water use only liquid soap and dry thoroughly with kitchen roll. Refer to hand hygiene procedure | Hand hygiene prior to contact with patient |
| Expose catheter site | To enable observation of any discharge or meatal problems |
| Check for allergies latex etc. | To ensure client safety |
| Open outer packaging of the solution | Content |
| Decontaminate hands with alcohol hand gel or soap and water or soapy hand wipes | To prevent cross-infection |
| Apply apron and sterile gloves and place sterile dressing field under catheter site | To prevent cross-infection |
| Disconnect drainage bag from catheter. Connect solution to catheter and instil as per manufactures instructions | To enable administration |
| Disconnect the solution and reconnect a new drainage bag with chosen method of support | To allow urine drainage |
| Dispose of equipment using appropriate waste stream | To prevent cross-infection |
| Remove and dispose of gloves and apron in the appropriate waste stream. Decontaminate hands with alcohol hand gel, soap and water or soapy hand wipes | To prevent cross-infection |
| Document procedure including reason and outcome | To meet legal requirements |
| Discuss result with patient | To involve and empower patient |
11.8 Appendix H Indwelling urinary catheterisation assessment
Catheterisation is recognised as a skilled aseptic non-touch procedure that requires appropriate training and competences. When considering catheterisation nurses must follow the Royal College of Nursing (RCN) guidelines for nurses (2019) on catheter care.
| Indication | Action |
|---|---|
| Drainage |
|
| Investigations | Urodynamics x-ray investigations |
| Instillation | To irrigate the bladder For the instillation of drugs |
| Management of incontinence | For end of life patients, where catheterisation allows patients to cope with pain, frequency of micturition and maintenance of dignity facilitating continence and maintain skin integrity (when all conservative treatment methods have failed) |
11.8.1 Acute retention
Retention of urine can be acute or chronic. Chronic retention can be associated with either low or high intravesical pressure
Acute retention:
- presents with inability to pass urine for
- several hours
- usually associated with lower abdominal
- pain
- bladder is visible and palpable
- bladder is tender on palpation
When to use with caution:
- recent urethral surgery
- unexplained haematuria
- history of false passages or strictures
- pelvic or perineal trauma-fractured pelvis
- urinary infection
11.8.2 Chronic retention
Chronic retention is usually relatively painless. High pressure chronic retention can cause hydro nephrosis and renal impairment.
Chronic retention:
- can present as late-onset enuresis
- may also present with hypertension
- low pressure chronic retention presents with symptoms of bladder outflow obstruction
- need to perform neurological examination to exclude disc prolapse
- patients with chronic retention and renal impairment need urgent urological assessment
11.8.3 Contra indications for urethral catheterisation
- Lack of consent.
- Urethral stricture or obstruction.
- Undiagnosed haematuria.
- History of difficult urethral catheterisation-including malformed genitalia.
- Previous failed attempt.
- Radical prostatectomy within 3 months.
- Mental health or cognitive status may affect the patient’s ability to give consent or cope with catheter care. Confused patients may attempt to forcibly remove the catheter which could lead to urethral trauma and infection.
- The patient may have dexterity and mobility problems which may affect the ability to manage the catheter and drainage systems. Carer availability must also be considered to undertake catheter care in these circumstances.
11.8.4 HOUDINI
When deciding if a catheter is still required, staff should consider the HOUDINI nurse led protocol which considers acceptable rationales for patients being catheterised.
- Haematuria, visible haematuria.
- Obstruction, urinary retention.
- Urology, surgery or retention.
- Decubitus ulcer, an open sacral or perineal wound in patient who is incontinent.
- Input or output, fluid monitoring, (should only be used in the acute setting).
- Nursing end of life, for comfort.
- Incontinence, only when all other alternative methods of management have been exhausted (this may include aids or ISC and discussion with the specialist continence sister.
If the answer to all of the above is “no”, then the patient should be referred to the specialist continence service for a trial without catheter as soon as possible to reduce the risks of catheter associated urinary tract infections (CAUTI’s).
The reason for catheterisation should be reviewed at each catheter intervention to see if it can be removed
11.9 Appendix I Catheter risk assessment what you need to know
11.9.1 Questions to consider in catheter care
- Is the catheter in use, is it necessary? Follow HOUDINI protocol artificial.
- What type of catheter is in use? Long-term, short term, open tip, Tieman tip.
- Is a closed drainage system maintained?
- Is catheter inserted using dressing pack, catheter tray with catheter attached to the leg bag?
- Is the catheter secured to the patient’s body to prevent urethral tension?
- How secure is it? for example, Straps, fixation device.
- Is the bag below the level of the bladder? (except the belly bag).
- Is the tubing secured from the bed or chair to prevent pulling on entire system? (night bag stand).
- Is the bag hanging free without touching the floor?
- Does the patient have an individualised urinal or jug with their name on it for emptying the bag?
11.9.2 Patients where associated catheterisation infection risks may be of serious nature
- Heart valve.
- Heart defect.
- Immuno-suppressed.
- Organ transplant.
- Faecal incontinence.
- One kidney.
- Since having a catheter the patient has had a urinary infection (high risk of further infections, potential to become resistant to).
11.9.3 Risk factors which increase the serious complications associated with catheter related infections
- The patient has been in hospital in the last 12 months, exposed to cross infection.
- The patient has taken antibiotics in the last 6 months.
- Pregnancy.
- Over 65 years of age increased vulnerability.
- Diabetes.
- More than six medications indicative of compromised health status.
- Chemotherapy within the last six months.
- Taking steroids.
- One functioning kidney, currently taking antibiotics for a UTI.
- Underlying renal tract abnormalities.
- At least one UTI since using a catheter.
- Chronic wounds requiring dressing will potentially cross-infect the catheter and drainage system.
11.9.4 Factors that could identify the risk of failing a trial without catheter in men
- Prostate.
- Previous episodes of acute episodes of retention.
- Over the age of 70 years old.
- Previous failed trial without catheter.
- Not on alpha blockers (tamusolisin).
11.9.5 Factors which identify underlying health problems
- Previous difficulty in catheter insertion and, or removal.
- History of catheter blockage.
- Catheter has fallen out.
- Bypassing.
- Patient is currently on antibiotics.
- Pain, discomfort and discharge associated with catheter usage.
11.9.6 Risks of haematuria include
- Medication such as aspirin or warfarin.
- Recent catheter related trauma.
- Recent urinary tract surgery.
- Known bladder or prostate cancer.
- Meatal bleeding observed by patient.
- Blood clots have been observed by the patient.
11.9.7 Allergy risks related to catheterisation to consider include
- Latex.
- Soap.
- Medication, for example, Lidocaine.
11.9.8 Risk factors which may increase urinary output when in supine position (important when considering flow rates or trial without catheter when patient is upright) include
- Heart disease.
- Diuretics.
- Postural oedema.
- Hypertension.
11.10 Appendix J Catheter selection
11.10.1 Plastic or PVC
Advantage:
- large internal diameter allows good drainage postoperatively
Disadvantage:
- rigid and inflexible, may cause urethral discomfort
Duration of catheter:
- 7 days
11.10.2 PTFE, Teflon coated latex
Advantage:
- smoother outer surface, reduces tissue damage and more resistant to encrustations than pure latex
Disadvantage:
- unsuitable for people with latex allergies, please refer to appendix H risk assessment
Duration of catheter:
- 28 days
11.10.3 Silicone Elastomer coated latex
Advantage:
- smooth internal and external surfaces, may reduce potential for encrustation over pure latex
Disadvantage:
- unsuitable for people with latex allergies, please refer to appendix I risk assessment
Duration of catheter:
- 12 weeks
11.10.4 Hydrogel coated latex
Advantage:
- more compatible with body tissue, less trauma, low surface friction, improved patient comfort
Disadvantage:
- unsuitable for people with latex allergies, please refer to appendix I risk assessment
Duration of catheter:
- 12 weeks
11.10.5 All Silicone
Advantage:
- they have a slightly wider lumen than that of coated catheters; therefore should be considered if the patient is prone to blockage of their catheter, suitable for patients with a latex allergy
Disadvantage:
- silicone allows diffusion of water, balloons may therefore occasionally deflate in situ, causing the catheter to fall out
Duration of catheter:
- 12 weeks
11.11 Appendix K Acute chronic retention in males first time male pathway
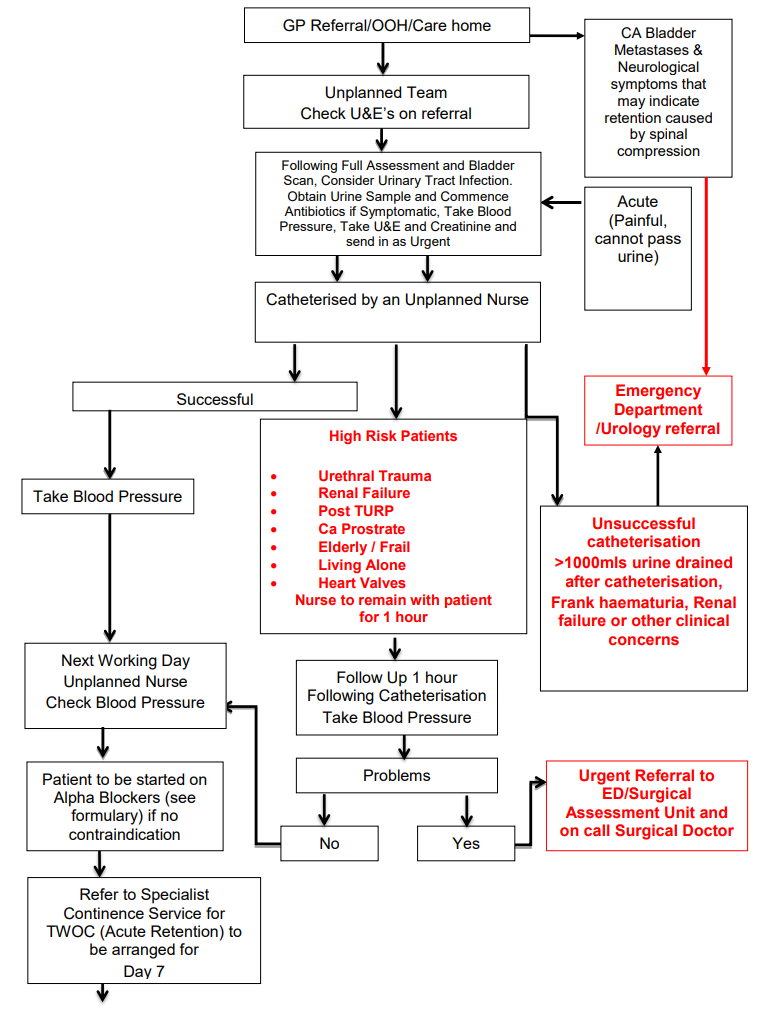
- GP Referral or OOH or care home:
- CA bladder metastases and neurological symptoms that may indicate retention caused by spinal compression
- emergency department or urology referral
- Unplanned team check U and E’s on referral.
- Following full assessment and bladder scan, consider urinary tract infection. Obtain urine sample and commence antibiotics if symptomatic, take blood pressure, take U and E and creatinine and send in as urgent (acute (painful, cannot pass urine).
- Catheterised by an unplanned nurse.
11.11.1 Catheterisation unsuccessful
- Unsuccessful catheterisation greater than 1000mls urine drained after catheterisation, frank haematuria, renal failure or other clinical concerns.
- Emergency department or urology referral.
11.11.2 High risk patients
These include patients with:
- urethral trauma
- renal failure
- post TURP
- ca prostrate
- elderly or frail
- living alone
- heart valves
- nurse to remain with patient for 1 hour
- follow Up 1 hour following catheterisation take blood pressure
- Any problems?
- Yes, urgent referral to ED or surgical assessment unit and on call surgical doctor
11.11.3 Catheterisation successful
- Successful, take blood pressure.
- Next working day unplanned nurse check blood pressure.
- Patient to be started on alpha blockers (see formulary) if no contraindication.
- Refer to specialist continence service for TWOC (acute retention) to be arranged for day 7.
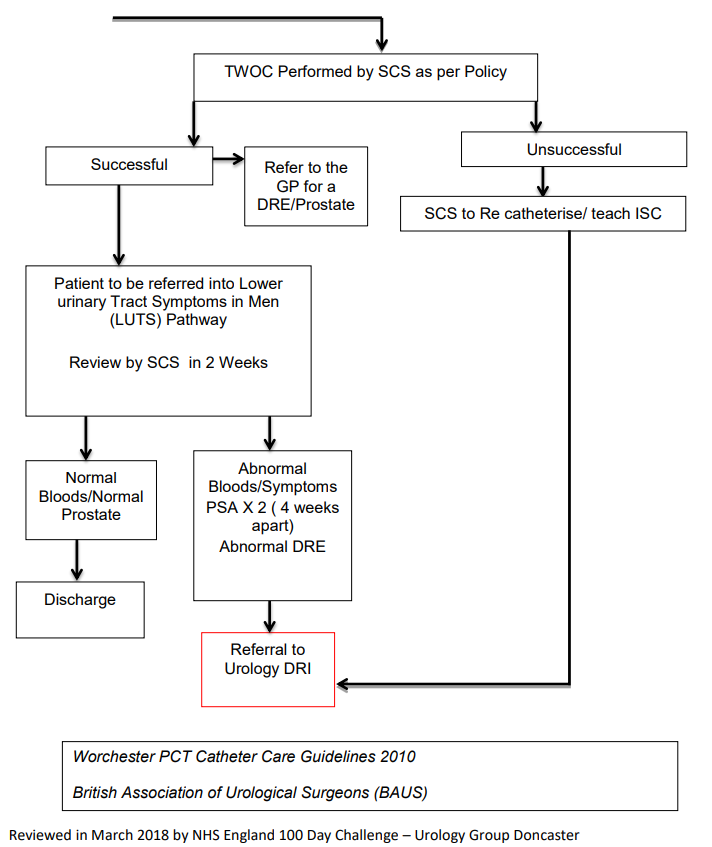
- TWOC performed by SCS as per policy.
11.11.3.1 TWOC unsuccessful
- SCS to re catheterise or teach ISC.
- Referral to urology DRI.
11.11.3.2 TWOC successful
- Successful, refer to the GP for a DRE or prostate.
- Patient to be referred into lower urinary tract symptoms in men (LUTS) pathway review by SCS in 2 weeks.
- normal bloods or normal prostate, discharge
- Abnormal bloods or symptoms PSA 2 times (4 weeks apart) abnormal DRE, Referral to urology DRI
11.12 Appendix L Intermittent self catheterisation 3-day diary
11.13 Appendix M Changing a leg bag procedure
Equipment:
- sterile dressing pack containing galipots or an indented plastic tray, low-linting swabs or medical foam, gloves (sterile and non-sterile), sterile field and disposable bag
- new leg bag
- receptacle for old leg bag
- appropriate fixing to support leg bag
| Action | Rationale |
|---|---|
| Explain and discuss the procedure with the patient Use suitable private area | To ensure the patient understands the procedure and gives informed consent. To ensure privacy |
| Decontaminate hands using alcohol hand gel or liquid soap and water or for community settings soapy hand wipes can be used followed by alcohol hand gel. Note, If in patients own home and hands are decontaminated with soap and water use only liquid soap and dry thoroughly with kitchen roll. Refer to hand hygiene procedure | Hand hygiene prior to contact with patient |
| Put on apron, open sterile dressing pack and apply sterile gloves | To prevent cross-infection |
| Place sterile towel under connection between catheter and bag | To prevent cross-infection |
| Separate leg bag from catheter using a gauze swab and insert the new leg bag immediately without touching the end of the new leg bag | To reduce risk of contamination and to minimise the length of time drainage system is broken |
| Secure new leg bag with chosen method of support | To prevent tension on the catheter by weight of urine |
| Risk assess the need to wear goggles. Empty urine in the night bag into sluice or toilet and discard night bag in appropriate waste stream | To prevent cross-infection, to prevent splash back |
| Dispose of equipment using appropriate waste stream | To prevent cross-infection |
| Remove and dispose of gloves and apron in the appropriate waste stream. Decontaminate hands with alcohol hand gel, soap and water or soapy hand wipes | To prevent cross-infection |
| Document the amount of urine drained and the date of the next change in the patients’ records. Document the date of change on the catheter bag | Comprehensive data for protection of nurse carrying out procedure and patient receiving the procedure |
11.14 Appendix N Emptying a catheter bag procedure
Equipment:
- non-sterile gloves
- apron
- disposable pulp receptacle or jug (single use) Note, patients own home jug (kept for this purpose only)
- gauze or tissue
| Action | Rationale |
|---|---|
| Explain the procedure to the patient | To obtain consent and ensure the patient understands the procedure |
| Decontaminate hands using alcohol hand gel or liquid soap and water or for community settings soapy hand wipes can be used followed by alcohol hand gel. Note, if in patients own home and hands are decontaminated with soap and water use only liquid soap and dry thoroughly with kitchen roll. Refer to hand hygiene procedure | To prevent cross-infection |
| Put non-sterile gloves and apron on | To prevent cross-infection |
| Put pulp receptacle or jug under tap ensuring the tap does not come into contact with the jug. Open the tap and allow urine to drain until the bag is empty | To prevent cross-infection and ensure complete emptying of the bag |
| Close the tap and clean with gauze or tissue | To prevent leakage and prevent cross-infection |
| Risk assesses the need to wear goggles. Dispose of urine in the sluice or toilet | Assess risk of splash back. To prevent cross-infection |
| Dispose of pulp receptacle using appropriate waste stream. Note, in patients own home, clean the jug with appropriate cleansing solution | To prevent cross-infection |
| Remove and dispose of gloves and apron in the appropriate waste stream. Decontaminate hands with alcohol hand gel, soap and water or soapy hand wipes | To prevent cross-infection |
| Record urine measurement in notes if required | To maintain accurate fluid balance |
11.15 Appendix O Single use night bag connecting procedure
Equipment:
- new single use night bag
- non-sterile gloves
- apron
- gauze
- catheter stand
| Action | Rationale |
|---|---|
| Explain procedure to patient | To ensure the patient understands the procedure and gives informed consent |
| Decontaminate hands using alcohol hand gel or liquid soap and water or for community settings soapy hand wipes can be used followed by alcohol hand gel. Note, If in patients own home and hands are decontaminated with soap and water use only liquid soap and dry thoroughly with kitchen roll. Refer to hand hygiene procedure | Hand hygiene prior to contact with patient |
| Put on apron and non-sterile gloves | To prevent cross-infection |
| Connect single use night bag to leg bag port, turn leg bag tap to open and ensure tubing is not kinked | To ensure free drainage from leg bag to night bag without breaking closed drainage system |
| Loosen leg bag supports and fix night bag to catheter stand on the floor or stand attached to the side of the bed. Decontaminate hands with alcohol hand gel, soap and water or soapy hand wipes | To facilitate drainage of urine and to aid patient comfort |
| Remove and dispose of gloves and apron in the appropriate waste stream | To prevent cross-infection |
| Document in the patients’ record that the night bag has been attached | Comprehensive data for protection of nurse carrying out procedure and patient receiving the procedure |
Note, for terminal patients who are nursed in bed or patients in the acute setting where the use of a leg bag is not required, a reusable night drainage bag may be attached directly to the catheter and changed every 7 days.
11.16 Appendix P My catheter passport NH598iii
11.17 Appendix Q Pad weighing instructions
Document control
- Version: 2.2.
- Approved by: Clinical policies review an approval group.
- Date approved: 4 October 2022.
- Name of originator or author: Team leader specialist continence service.
- Name of responsible individual: Senior specialist continence sister.
- Date issued: 7 October 2022 (amendment).
- Review date: March 2025.
- Target audience: All staff working in Doncaster area. Staff working in Rotherham and Scunthorpe, they will need to refer local guidelines.
Page last reviewed: December 10, 2024
Next review due: December 10, 2025
Problem with this page?
Please tell us about any problems you have found with this web page.
Report a problem