Contents
1 Aim
This standard operating procedure (SOP) is to ensure that all medical colleagues and clinicians within the child and adolescent mental health service (CAMHS) have a full understanding of the expectations placed on them whilst a child or young person is placed in a tier 4 establishment. This includes face to face visits, communication with the tier 4 unit and communication with the child or young person and their carers or family.
2 Scope
The SOP is for use by all CAMHS clinicians and medical colleagues within the children’s care group.
3 Link to overarching policy
This SOP should be read in conjunction with the following trust policy:
4 Procedure
Any child and young person that has been admitted to a tier 4 unit via a planned or unplanned route needs to have the stability and security of knowing the frequency of visits from their care coordinator or lead worker and their consultant psychiatrist.
For young people not under the CAMHS Eating Disorder or CAMHS Intellectual Disability teams, an open referral to the Intensive Community Support team (CAMHS ICS) is required prior to admission alongside a named care coordinator or lead worker and a consultant psychiatrist. This is inclusive of young people open to the Early Intervention in Psychosis team (EIT). Whilst in tier 4, the CAMHS Intensive Community Support team should take the role of lead professionals for the duration of the admission. There may be cases where the CAMHS Intensive Community Support team may support cases open to the CAMHS Eating Disorder or CAMHS Intellectual Disability teams if appropriate.
For young people not under CAMHS ICS, once a child or young person has been admitted it is the responsibility of the care coordinator or lead worker to alert their team lead or clinical lead to the admission. The relevant team lead or clinical lead, upon being informed of the admission, will allocate another worker to co-work with the child or young person and to ensure that the tier 4 units have increased access to a named CAMHS Clinician. It is the responsibility of both clinicians to ascertain who will attend and liaise with the tier 4 unit.
In the case of a child or young person open to the CAMHS ICS team, as they assume the role of the co-worker and as lead professionals, they will be expected to attend and liaise with both the tier 4 unit and community CAMHS clinicians and any other professionals involved in care.
The care coordinator or lead professional needs to complete the details of the admission on SystmOne (appendix A)
For a child or young person open to the CAMHS ICS Team, there is an expectation that the team will attend weekly ward MDTs either in person or virtually to ensure regular community representation within care discussions and to ascertain the patient’s progress or deterioration and adapt the local care plan or crisis plan to replicate work that is being done at the unit. Pertinent information from MDTs and any other meetings attended by community CAMHS during the time of a child or young persons admission to tier 4 should be documented within the SystmOne notes of the child or young persons electronic patient record, including any actions given to the CAMHS care coordinator/lead professional and CAMHS consultant.
At the child and young person’s admission, first care programme approach (CPA) review, the care coordinator or co-worker will attend the meeting to ensure collaboration with the Tier 4 unit on the patient’s care plan, risk assessment, crisis plan, contingency plan and future discharge planning. If both named workers are unable to attend this meeting, then either the consultant psychiatrist or a representative from CAMHS will attend (this meeting may be set up for face to face or over virtual media).
It is expected that either the care coordinator or co-worker will actively engage in each CPA review, or where there are significant changes in the patient’s presentation, they would be expected to attend to support a review of the situation. If the care coordinator is unable to attend in person, then consideration needs to be given to alternative forms of attendance and communication such as virtually by Microsoft Teams and conference calls. The care coordinator or co-worker when visiting the patient should also view the patient’s electronic care records to ensure that both the tier 4 care plan and the local CAMHS care plan are working in collaboration; and update the local record accordingly.
The child or young person’s leave from the unit needs to be managed collaboratively by the tier 4 unit and local CAMHS service, where a local CAMHS service has not been made aware of home leave; this would need to be reported directly to their team lead or clinical lead and CYP provider collaborative so they can take appropriate action.
The consultant psychiatrist will liaise with the consultant psychiatrist at the tier 4 unit around the child or young person’s treatment and medication plan, to ensure that on discharge both parties are in agreement with the plan. The consultant psychiatrist where possible should attend CPA reviews (which may be face to face or virtual meetings)
There is also an expectation that the consultant psychiatrist will attend any discharge planning meetings, to ensure that the Community team have a robust and appropriate support plan in place. If in unexpected circumstances the consultant psychiatrist cannot attend the scheduled discharge planning meeting, then a telephone conference call or virtual meeting that the consultant psychiatrist can attend should be arranged as soon as possible.
Outside these meetings, the care coordinator or co-worker should make at minimum fortnightly contact with the tier 4 unit by telephone or virtually to ascertain the patient’s progress or deterioration and adapt the local care plan or crisis plan to replicate work that is being done at the unit. If it is not possible for weekly ward MDTs to attended requests should be made to the unit for weekly progress reports to be sent to CAMHS clinicians and the local CAMHS consultant psychiatrists for updates.
If the local CAMHS consultant psychiatrist disagrees with specific clinical plans and interventions treatments initiated by the tier 4 unit, then a conversation must occur, consultant to consultant. This may result in a visit to the unit by the local CAMHS consultant psychiatrist to gather further information. If the care coordinator or co-worker has any concerns surrounding certain clinical plans and interventions or treatments this information will need to be passed to the local CAMHS consultant psychiatrist for advice.
During the child or young person’s admission the care coordinator or co-worker needs to have regular contact with the child or young person’s carers or family to make sure they are updated with child or young person’s care, and if any concerns are raised these are reported to the team lead or clinical lead manager. The family should be made aware of any changes to local care planning; this may include transferring a child or young person closer to their local community. Any changes to the family’s position may need to be included in the child or young person’s care plan, for example where a family cannot have the child or young person back home. Any discharge plans and future care plans for those children or young people detained under Section 3 of the Mental Health Act should consider the requirements of Section 117 the aftercare needs of the child/young person and liaise with Local Authorities to support. (refer to the trust’s section 117 policy for further information).
4.1 Long term placements, extending beyond 6 months
Where a child and young person is likely to be placed in a tier 4 or specialist placement, for a period extending beyond 6 months, then liaison with the unit and frequency of contacts do not need to be as often as stated above. However, there is an expectation that contact should occur monthly to the unit and the child or young person (as appropriate). In cases where the child or young person is open to the CAMHS team, the plan of support in terms of liaising with the unit and frequency of contacts with the child or young person should not change.
The frequency and level of contact needs to be documented in the child and young person’s care plan, ensuring all relevant parties agree with these contact arrangements. It is still expected that active representation by the care coordinator or co-worker is provided to each CPA review, delegation of who attends may be flexible, especially in smaller specialist teams such as intellectual disability. Where face to face representation cannot occur then other forms of communication need to be explored such as virtually by Microsoft Teams or conference calls.
4.2 Working together to safeguard children 2023
Anyone who has concerns about a child’s welfare should consider whether a referral needs to be made to local authority children’s social care and should do so immediately if there is a concern that the child is suffering significant harm or is likely to do so. Where a child is admitted to a mental health facility, practitioners should make a referral to local authority children’s social care. When practitioners refer a child, they should include any information they have on the child’s developmental needs, the capacity of the child’s parents, carers, or family network to meet those needs and any external factors that may be undermining their capacity to parent. This information may be included in any assessment, including an early help assessment, which may have been carried out prior to a referral into local authority children’s social care. An early help assessment is not a prerequisite for a referral but where one has been undertaken, it should be used to support the referral.
When making referrals to social care, both community professionals and the tier 4 unit should discuss this referral with the young person’s family/carers prior to making the referral and ensure consent is given if it is safe and appropriate to do so.
4.3 Section 85 Children Act (1989)
Where a child and young person has been placed in a tier 4 unit for more than 3 months the local children services need to be made aware to undertake section 85 duties. It is the responsibility of the care coordinator or co-worker and the tier 4 unit to ensure that the relevant local authority is aware of the admission (see appendix B).
4.4 Care, education and treatment review (CETR) process
For children and young people with a diagnosis of intellectual disability or autism, a care, education and treatment review (CETR) or local area emergency protocol (LAEP) meeting must be completed prior to any admission. The relevant local ICB need to ensure that they invite all appropriate agencies and distribute all related information. It is the responsibility of the local ICB to ensure CETR and LAEP meetings are arranged and managed accordingly.
For children or young people that have been through the CETR process, the CETR is reviewed upon a tier 4 admission, this is the responsibility of the CYP provider collaborative and tier 4 unit.
Should a young person be given a neurodiverse diagnosis while in a tier 4 unit, it is the role of the lead professional to notify and make a referral to the ICB care navigators.
4.5 Conflict resolution of tier 4 issues
All initial problems should be passed to the team lead or clinical lead to liaise with the appropriate tier 4 unit and the CYP provider collaborative if appropriate. If at this point issues cannot be resolved, then the manager will pass the information on to the appropriate CAMHS service manager. If problems continue to persist and a resolution has not been found, then this will continue up to the children’s care group director or care group director of nursing.
4.4.1 Conflict resolution process
- Care coordinator or co-worker.
- Team lead or clinical lead.
- Service manager.
- Children care group director or care group director of nursing.
5 Appendices
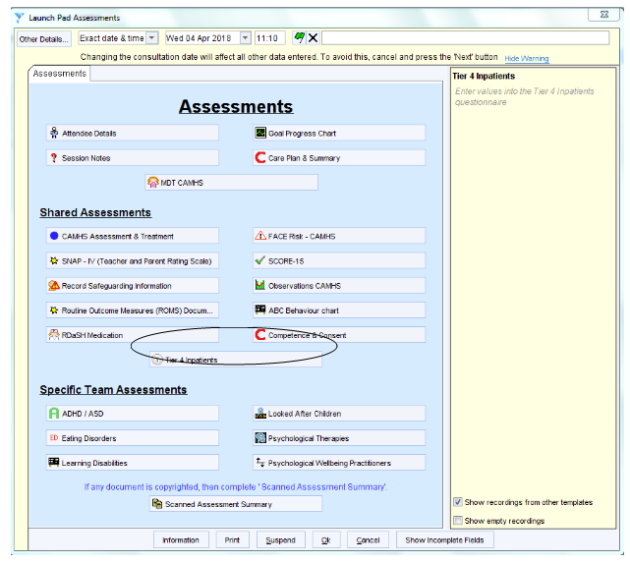
5.1 Appendix A SystmOne tier 4 form
CAMHS launchpad assessment window.
5.2 Appendix B Section 85 and 86 Children Act (1989) notifications to children’s social care
Sections 85 and 86 of the Children Act 1989 were introduced to ensure that children who are accommodated by a health agency, local education authority, care home or independent hospital for a consecutive period of at least three months are brought to the attention of children’s social care. Such children are potentially vulnerable by virtue of their being accommodated outside the family.
Upon notification that a child from their area is living in such arrangements, Children’s social care can assess whether the child’s welfare is being adequately safeguarded and promoted and whether any additional services or interventions should be offered to the child and their family.
As sections 85 and 86 only apply to those children who are accommodated for a consecutive period of at least three months, the provisions do not apply to children placed on a term-to-term basis in boarding school where they return home during the school holidays.
It is a requirement of the accommodating authority to notify children’s social care for a child who would normally be resident within that local authority area if they are providing accommodation for a consecutive period of at least three months or if they have the intention of providing accommodation for such a period.
5.2.1 Legal requirements
5.2.1.1 Section 85 Children Act (1989)
- Where a child is provided with accommodation by any Local Health Board, Special Health Authority, Primary Care Trust, National Health Service Trust, NHS Foundation Trust or local education authority (“the accommodating authority”):
- for a consecutive period of at least three months
- with the intention, on the part of that authority, of accommodating him for such a period, the accommodating authority shall notify the responsible authority.
- Where subsection (1) applies with respect to a child, the accommodating authority shall also notify the responsible authority when they cease to accommodate the child.
- In this section “the responsible authority” means:
- the local authority appearing to the accommodating authority to be the authority within whose area the child was ordinarily resident immediately before being accommodated
- where it appears to the accommodating authority that a child was not ordinarily resident within the area of any local authority, to local authority within whose area the accommodation is situated.
- Where a local authority has been notified under this section, they shall:
- take such steps as are reasonably practicable to enable them to determine whether the child’s welfare is adequately safeguarded and promoted while he is accommodated by the accommodating authority
- consider the extent to which (if at all) they should exercise any of their functions under this Act with respect to the child.
5.2.1.2 Section 86 Children Act (1989)
- Where a child is provided with accommodation in any care home or independent hospital:
-
- for a consecutive period of at least three months
- with the intention, on the part of the person taking the decision to accommodate him, of accommodating him for such period
the person carrying on the home shall notify the local authority within whose area the home is carried on.
-
- Where subsection (1) applies with respect to a child, the person carrying on the home shall also notify that authority when he ceases to accommodate the child in the home
- Where a local authority has been notified under this section, they shall:
- take such steps as are reasonably practicable to enable them to determine whether the child’s welfare is adequately safeguarded and promoted while he is accommodated in the home
- consider the extent to which (if at all) they should exercise any of their functions under this Act with respect to the child
- If the person carrying on any home fails, without reasonable excuse, to comply with this section he shall be guilty of an offence.
- A person authorised by a local authority may enter any care home or independent hospital within the authority’s area for the purpose of establishing whether the requirements of this section have been complied with.
- Any person who intentionally obstructs another in the exercise of the power of entry shall be guilty of an offence.
- Any person exercising the power of entry shall, if so required, produce some duly authenticated document showing his authority to do so.
- Any person committing an offence under this section shall be liable on summary conviction to a fine not exceeding level 3 on the standard scale.
Document control
- Version: 4.
- Unique reference number: 11.
- Date ratified: 3 December 2024.
- Ratified by: Clinical policies review and approval group.
- Name of originator: Surgical CG administration team general manager.
- Name of responsible individual: Children’s care group director.
- Date issued: 18 December 2024.
- Review date: 31 December 2027.
- Target audience: All clinical staff in children and young people’s mental health service across the trust.
Page last reviewed: January 08, 2025
Next review due: January 08, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.