What is plantar fasciitis?
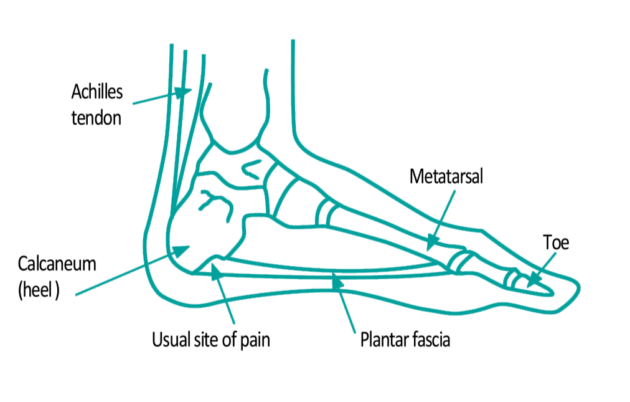
Plantar fasciitis means inflammation of the plantar fascia. The Plantar Fascia is a strong fibrous band of tissue (like a ligament) that stretches from the heel bone (calcaneum) and fans out towards the toes. It supports the arch of the foot. Pain comes from microscopic tears within the plantar fascia. Symptoms can resolve with time.
What are the symptoms of plantar fasciitis?
Pain on the underside of the heel is the main symptom. Usually one spot is found as the main area of pain and may be tender to touch.
The pain tends to be worse when getting out of bed in the morning and when taking the first few steps after resting. It may ease with gentle exercise, but increased activities or being on the feet for a long period of time may worsen the pain towards the end of the day. Resting the foot usually eases the pain.
Sudden stretching of the sole of the foot, for example walking upstairs or on tip-toes, may make the pain worse. Some people may limp with the pain. It is also possible to have plantar fasciitis in both feet at the same time.
How common is plantar fasciitis?
Around 1 in 10 people will get plantar fasciitis at some time in their life. Although it can occur at any age, it is most common in people between the ages of 40 to 60 years. It is twice as common in women than men.
It is also common in athletes.
What causes plantar fasciitis?
It is caused by repeated tension on the plantar fascia causing microscopic tears in the tissue. The injury is usually near where the plantar fascia attaches on to the heel bone, but can also occur in the arch.
The plantar fascia is more likely to become injured in certain situations. For example, if you are standing on your feet for a long period of time, or if you do lots of walking and running etc.
If you are overweight this will apply added strain on your plantar fascia.
Poor foot posture, for example very flat feet or very high arches will add extra strain on the plantar fascia.
If you have tight calf and hamstring muscles, this can reduce your ability to use your ankle joint effectively and make you more likely to damage the plantar fascia.
Sudden increases in activity levels or stretching of the sole. If you have changed the surface you are exercising on, for example running on the road instead of the track.
Wearing shoes with poor arch support or with poor cushioning can also lead to heel pain.
Heel spur
It is a common belief that the pain is due to a “spur” or bony growth from the heel bone (calcaneum). This is not always the case as many people have this bony heel spur, but not everybody with this has plantar fasciitis.
Treatments
An assessment will identify the most likely cause of the problem. The treatment programme will vary depending upon the cause. All treatments are aimed at decreasing the stress on the plantar fascia and reducing inflammation. The fascia tissue heals quite slowly. However a combination of the following treatments may help to speed recovery.
Non-invasive treatments are used in the first case, these include:
Rest
Use pain as your guide. If the foot is painful, rest it. Avoid running, excessive walking or standing.
Cold treatment
Freeze a small bottle of water or can of beans. Keep your socks on and roll the cold can or bottle under the arch and heel of the foot for 5 to 10 minutes. This can be repeated up to 3 times a day.

This is a good exercise because not only does it stretch and massage the plantar fascia, it also provides cold therapy to the inflamed injured area.
Exercise programme
Calf stretches
Gastrocnemius stretch
Stand with feet parallel, hip width apart, take a step forward. Ensure your back foot is flat to the floor and is facing forward. Bending your front knee take most of your weight on the leading foot. Hold for 20 seconds.
Repeat three times, three times daily.

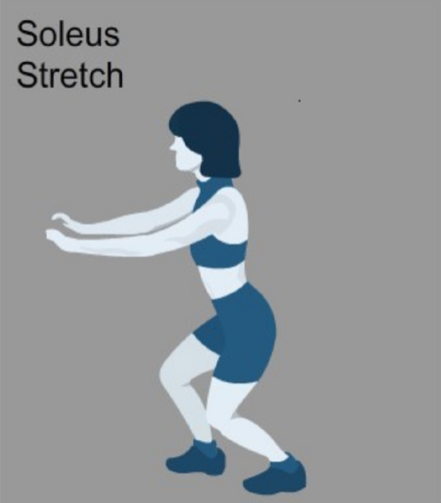
Soleus stretch
Stand in the same position as above but this time bend both the front and the back knee. Hold for 20 seconds.
Repeat three times, three times daily.
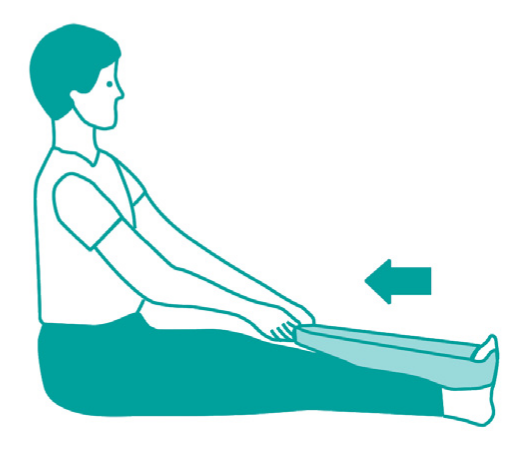
Towel stretch
Sit on the floor or bed with your legs stretched out in front of you. Loop a towel around the injured foot. Hold your foot straight and slowly lean forwards. Hold for 20 seconds then relax.
Repeat 10 times, once a day.
Foot strengthening exercises
Towel curls, marble pick-up and drawing letters of the alphabet with your toes will strengthen the foot.
Towel curls
Place a towel on the floor, with the foot on the towel; pull the towel towards the body by curling up the toes.
Marbles pick-up
Place a few marbles on the floor near a cup. Keep the heel on the floor and use the toes to pick up the marbles and drop them into the cup.
Alphabet exercise
Keeping the heel placed in one position on the floor, with your toes draw the range of alphabet letters from A to Z in upper and lower case.
Footwear
Do not walk barefoot on hard surfaces. Wearing hiking shoes or trainers with good support, especially around the heel and under the arch, will help. Shoes should have laces to keep the foot in place. A small heel is acceptable. You should avoid wearing thin soled, worn out, or distorted shoes.
Orthoses
These are insoles or shoe inserts that may be prescribed to you by the podiatrist. These devices will provide support for your foot and reduce the strain borne upon the plantar fascia. If you have been provided with insoles, use them as much as possible.
Medication
Anti-inflammatory gel can be useful in some cases. It is advisable to consult with your GP or pharmacist to see if it is appropriate for you to use them.
Further treatments
Further invasive treatments are only considered when other treatments do not work. These include:
- steroid injection, this aims to reduce inflammation and pain in the tissue
- surgery, this is rarely required for plantar fasciitis and is only considered when all forms of conservative treatment fail
Contact podiatry foot protection
Document control
- Document reference: DP7831/07.17.
- Date reviewed: April 2017.
Page last reviewed: October 17, 2024
Next review due: October 17, 2025
Problem with this page?
Please tell us about any problems you have found with this web page.