Contents
- Introduction
- Purpose
- Scope
- Responsibilities, accountabilities and duties
- Procedure or implementation
- Deprivation of liberty in settings other than a care home or hospital, judicial deprivation of liberty
- Training implications
- Monitoring arrangements
- Equality impact assessment screening
- Links to any other associated documents
- References
- Appendices
1 Introduction
The aim of the Rotherham, Doncaster and South Humber NHS Foundation Trust (RDASH) deprivation of liberty policy is to clearly state an agreed approach to identifying a deprivation of liberty and the appropriate and effective use of the deprivation of liberty safeguards (DoLS).
This policy should be underpinned by the Mental Capacity Act 2005 (MCA); the MCA Code of Practice (2007) and the Deprivation of Liberty Safeguards (DoLS) Code of Practice (2009), which serves as an addendum to the MCA Code of Practice. It is not a substitute for the act and the codes of practice, to which all professionals must adhere.
This policy assumes a knowledge and understanding of the MCA Mental Capacity Act 2005 policy and it should be read in conjunction with other policies.
2 Purpose
The purpose of this policy is to provide staff working in or with the trust with guidance about identifying a deprivation of liberty and how to seek authorisation.
It outlines the key responsibilities and expectations of the trust in respect of the use of DoLS, specifically the process which needs to be followed in order for RDaSH to meet its legal obligations as a managing authority in ensuring that any deprivation of a person’s liberty are authorised and lawful.
The trust is committed to ensuring that all people who are using our services are treated with dignity and respect and those individuals and their families or carers receive appropriate care and support.
3 Scope
Patients aged 16 and over on the trust’s inpatient wards or resident of a registered community home, who have been identified as:
- lacking the capacity to consent to their admission
- lacking the capacity to make an informed decision about their proposed care and treatment whilst under the care of the trust and
- are under continuous supervision and control and not free to leave
In circumstances where there is a deprivation of their liberty on an inpatient ward or community home and the Mental Health Act 1983 (MHA) does not apply the DoLS will be required to ensure that the deprivation is lawful and does not constitute a breach of the person’s human rights.
4 Responsibilities, accountabilities and duties
The trust is responsible for ensuring where patients aged 18 and over are admitted to an inpatient ward or a registered care home and are being deprived of their liberty, the deprivation is authorised in accordance with the law under DoLS.
Staff working with people 16 and over whom they believe may be deprived of their liberty in a setting other than a care home or hospital should notify the care provider and the commissioners of the care that authorisation is needed by the appropriate legal procedure in order to safeguard the person.
5 Procedure or implementation
5.1 Determining deprivation of liberty
On the 19 March 2014 the Supreme Court handed down its judgment in the case of P v Cheshire West and Chester Council and P and Q v Surrey County Council (2014) UKSC 19. The judgment is significant in the determination of whether arrangements for the care and treatment of an individual lacking capacity to consent to those arrangements amount to a deprivation of liberty.
5.1.1 “The acid test”
The key point arising from the supreme court judgment was the introduction of a revised test to determine whether a deprivation of liberty is occurring known as the “acid test”.
The two questions which now must be applied are:
- is the person subject to continuous supervision and control? continuous supervision and control refers to oversight even when the patient is not in the line of sight, it must amount to supervision and have a clear element of control
And:
- is the person free to leave? Free to leave, the person may not be asking to go or showing this in their actions, but the important factor is how staff would react if that person did try to leave or if a relative or friend asked to remove them
For a person to be deprived of their liberty all three elements must apply.
5.1.2 No longer relevant
The supreme court ruled that the following factors are no longer relevant in determining whether a patient is deprived of their liberty:
- the person’s compliance or lack of objection
- the relative normality of the placement (whatever the comparison made)
- the reason or purpose behind a particular placement
5.1.3 Capacity to consent
Where there is doubt about a patient’s capacity to give informed consent to being admitted to an inpatient ward or to reside in a RDaSH community home to receive care and treatment, staff involved in admitting the person should ensure that:
- a formal assessment of capacity has been undertaken and documented in relation to consent to admission on form MCA1 and
- where the patient lacks capacity to consent to admission a decision is made in their best interest interests and there is evidence of this recorded on form MCA2
5.1.4 Applying the acid test
Where it is established that the patient lacks the capacity to consent to being admitted to:
- an inpatient ward
- RDaSH community home
The assessing clinician must then establish whether the person is being deprived of their liberty by applying the “acid test” detailed above (5.5.1).
Where a potential deprivation of liberty is identified, a full exploration of the alternative ways to providing the care and treatment should be undertaken, in order to identify any less restrictive way of providing the care which will avoid a deprivation of liberty.
5.2 Legal authority to admit or be placed to receive care and treatment
Where it has been determined that a patient is being deprived of their liberty, and there is no less restrictive way of providing the necessary care and treatment the deprivation must be authorised in accordance with one of the following legal regimes:
- detention under The Mental Health Act 1983 (MHA) For those patients where the criteria for detention under the MHA applies (Refer to the appropriate MHA)
- authorisation under the Deprivation of Liberty Safeguards (DoLS) (schedule A1 to the MCA) For those patients in care homes and hospitals where the criteria is met under DoLS and who are not eligible to be detained under the MHA 1983 Staff should refer to appendix B for the standard operating procedure, deprivation of liberty safeguards
- an order of the Court of Protection (judicial deprivation of liberty) refer to the judicial deprivation of liberty (section 6 below)
- an order of the high court (Inherent Jurisdiction)
5.3 Deprivation of liberty in a psychiatric hospital setting, MHA or DoLS?
Where the patient lacks the capacity to consent to their admission and the circumstances of their admission will amount to a deprivation of their liberty the deprivation of liberty must be authorised.
If DoLS is being considered on a trust hospital ward once someone has been admitted then the patient will not be eligible if:
- they object to being admitted to hospital, or to some or all the treatment they will receive there for mental disorder
- they meet the criteria for an application for admission under section 2 or section 3 of the Mental Health Act 1983 (MHA) (unless an attorney or deputy, acting within their powers, had consented to the care and treatment to which the person is objecting)
However if a patient is:
- suffering from a mental disorder (within the meaning of the MHA) disregarding any exclusion for patients suffering with a learning disability
- needs to be assessed and, or treated in a hospital setting for that disorder or for physical conditions related to that disorder (and meets the criteria for an application for admission under sections 2 or 3 of the MHA)
- has a care treatment package that may or will amount to a deprivation of liberty
- lacks capacity to consent to being accommodated in the relevant hospital for the purpose of treatment
- does not object to being admitted to hospital, or to some or all the treatment they will receive there for mental disorder.
Then in principle a DoLS Standard Authorisation and detention under the MHA would both be available (subject to the assessments required for a DoLS authorisation, including the DoLS eligibility assessment). This is the one situation where the option of using either the MHA or DoLS exists. See appendix A.
For those patients where both detention under the MHA and a DoLS standard authorisation or a Court of Protection order are available, decision-makers should determine which legal framework is the more appropriate.
The choice of legal framework should never be based on a general preference for one regime or the other, or because one regime is more familiar to the decision maker than the other. In addition decision-makers should not proceed on the basis that one regime is generally less restrictive than the other. Both regimes are based on the need to impose as few restrictions on the liberty and autonomy of patients as possible. In the particular circumstances of an individual case, it may be apparent that one regime is likely to prove less restrictive. If so this should be balanced against any potential benefits associated with the other regime. Decision makers should consider if care can be delivered safely and effectively using DoLS instead of the MHA. DoLS cannot be used for the protection of others.
Both regimes provide appropriate procedural safeguards to ensure the rights of the person concerned are protected whilst being deprived of their liberty. Decision makers should not therefore proceed on the basis that one regime generally provides greater safeguards than the other. However, the nature of the safeguards provided under the two regimes are different and decision-makers will wish to exercise their professional judgement in determining which safeguards are more likely to best protect the interests of the patient in the particular circumstances of each individual case.
It is important that decision makers record their reasons for choosing one regime over another.
5.3.1 Objection
When considering whether a person is objecting the decision maker must take into account all the circumstances, so far as they are reasonably ascertainable. The reasonableness of the objection is not the issue. In many cases the person will be able to state their objection, in other cases the doctors and AMHP will need to consider the patient’s behaviour, wishes, feelings, views, beliefs and values, both present and past so far as they can be ascertained. If there is reason to think a patient would object, if able to do so, then the patient should be taken as objecting (MHA Code of Practice (2015) 13.51).
5.3.2 Deprivation of Liberty in hospital for the purpose of treatment for a mental disorder, options for authorisation
| Individual objects to the proposed accommodation in a hospital for care and or treatment, or to any of the treatment they will receive there for mental disorder | Individual does not object to the proposed accommodation in a hospital for care and or treatment, or to any of the treatment they will receive there for mental disorder | |
|---|---|---|
| Patient has capacity to consent to being accommodated in a hospital for care, and, or treatment | Only the MHA is available | The MHA is available informal admission might be appropriate. DoLS authorisation not available |
| Patient lacks capacity to consent to being accommodated in a hospital for care, and, or treatment | Only the MHA is available | The MHA is available. DoLS authorisation available |
5.3.3 DoLS eligibility, interface between DoLS and Mental Health Act 1983 (MHA)
A person is not eligible for a DoLS standard authorisation if they are:
- detained as a hospital in-patient under sections 2, 3, 4, 35, 36, 37, 38, 44, 45A, 47, 48 or 51 the MHA, case A
A person may be eligible for a DoLS standard authorisation if they are either:
- subject to hospital treatment regime but not detained and are required to live elsewhere, for example, patients on section 17 leave or subject to conditional discharge. Providing the deprivation of liberty does not conflict with a requirement imposed on them under the MHA, case B
- a supervised community treatment order providing the deprivation of liberty does not conflict with a requirement imposed on them under the MHA, case C
- who are subject to a guardianship order providing the deprivation of liberty does not conflict with a requirement imposed on them under the MHA or P objects not sure what this is? case D
- the person is within the scope of the MHA and could be detained in hospital and therefore an application could be made under section 2 or section 3 MHA and is an “objecting” mental health patient, case E
Staff should refer to appendix A for further guidance on the cases above.
5.3.4 Cases where neither the MHA nor DoLS can be used
There may be some instances in which neither the DoLS nor the MHA can be used to authorise the deprivation of a patient’s liberty in a psychiatric hospital.
Two are:
- where a patient is detained under the MHA but requires treatment for physical disorder to which they cannot consent and which will involve a further deprivation of liberty (for instance, force-feeding, enforced caesarean section)
- where there is a ‘stand-off’ that cannot be resolved between the decision-makers under the MHA and those under the MCA as to which route to use to authorise the deprivation of liberty. In either case, in order to ensure that the deprivation of liberty is lawful, it is necessary to make an application to the high court to invoke the inherent jurisdiction
6 Deprivation of liberty in settings other than a care home or hospital, judicial deprivation of liberty
6.1 Children and young people
There are likely to be a number of children and young people who are deprived of their liberty in various settings. However a deprivation of liberty will be lawful if authorised under one of the following statutes:
- section 25 of the Children Act 1989, which provides for the placement of looked after children in secure accommodation
- the Mental Health Act 1983
- the youth remand provisions of the Legal Aid, Sentencing and Punishment of Offenders Act 2012
- the custodial sentencing provisions of the Power of Criminal Courts (Sentencing) Act 2000
6.1.1 Children under 16
If a child under 16 is not under a formal care order, his or her parents can authorise a deprivation of liberty in the exercise of parental responsibility regardless of the child’s mental capacity, for example, in hospital.
If a child under 16 is under a formal care order, for example, looked after child under an interim or final care order who are deprived of their liberty the deprivation will need to be authorised by the family court, for example, foster home, children’s home, residential special school, boarding schools
6.1.2 16 and 17-year-olds
The courts have now confirmed that for 16 and 17-year-olds who are not under a formal care order and are deprived of their liberty and lack capacity to consent to the arrangements (or do have capacity and refuse) that those with parental responsibility cannot give valid consent. The deprivation will therefore have to be authorised by either:
- Mental Health Act 1983
- Court of Protection
For children and young people that are 16 and 17-year-olds who are “looked after” under an interim or final care order who are deprived of their liberty the deprivation will need to be authorised by the Court of Protection, for example, foster home, children’s home, residential special school, boarding schools, further education colleges with residential accommodation.
6.2 Deprivation of liberty in domestic settings
The Supreme Court held that a deprivation of liberty can occur in domestic settings where the State is responsible for imposing such arrangements. This will include a placement in a supported living arrangement, shared care and extra care housing in the community. DoLS is not available to authorise these cases, therefore any deprivation of liberty will require authorisation by the Court of Protection via the re X procedure.
6.3 Re X procedure
Following the Supreme Court judgment, the Court of Protection launched a new streamlined procedure in November 2014 with a view to dealing with an increased demand for such applications. This is known as the “re X procedure” and is supported by a new Court of Protection application form and a new practice direction.
The responsibility for seeking authorisation remains with those funding care in community setting (predominantly local authorities and Integrated care boards) who should ensure they have a procedure and policy in place for identifying those individuals who may lack capacity and be subject to a deprivation of liberty.
6.4 Staff responsibility in these cases (6.1 to 6.2)
It is not the trusts’ responsibility to seek authorisation for seeking authorisation for 16 and 17-year-olds living in the community.
If staff believe a 16 or 17-year-old is being deprived of their liberty, they should notify the commissions of the persons care of their concerns.
In order to assist staff a template letter of notification is available, see appendix C. The letter should be sent to the commissioners via email, password protected, copying in the MCA lead. A copy of the letter and the email should be kept on the patient’s case file.
7 Training implications
7.1 All qualified staff working on wards or in community homes where it is identified as essential to role (MCA Level 4)
- How often should this be undertaken: 3 years.
- Length of training: Half a day.
- Delivery method: MS Teams or face to face.
- Training delivered by whom: MCA Lead.
- Where are the records of attendance held: Electronic staff record system (ESR).
As a trust policy, all staff need to be aware of the key points that the policy covers and be able to access the DoLS standard operating procedure as further guidance. Staff can be made aware through a number of a variety of means such as:
- team meetings
- face to face training
- one to one meetings or supervision
- practice development days
- public website
- local induction
8 Monitoring arrangements
8.1 Training
- How: Training records.
- Who by: MHA or MCA training officer.
- Reported to: Mental health legislation committee.
- Frequency: Annual.
8.2 Policy implementation
- How: Audit.
- Who by: Mental Capacity Act lead.
- Reported to: Mental health legislation committee.
- Frequency: Annual.
9 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
9.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
9.1.1 How this will be met
There is no requirement for additional consideration to be given with regard to privacy, dignity or respect.
9.2 Mental Capacity Act
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals’ capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
9.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the principles of the Mental Capacity Act 2005 (section 1).
10 Links to any other associated documents
- MCA Mental Capacity Act 2005 policy
- Advance statements and advance decisions to refuse treatment policy
- Reducing restrictive interventions (RRI) policy (formerly PMVA policy)
- Consent to care and treatment policy
- Mental health act policies
- Safeguarding adults policy
- Records management policy
11 References
The MCA applies in conjunction with other legislation, under which health and social are staff have obligations relating to people who may lack capacity. See links below:
- Mental Capacity Act 2005 (opens in new window).
- Mental Capacity Act Code of Practice (opens in new window).
- The Mental Capacity (Deprivation of Liberty, Standard Authorisations, Assessments and Ordinary Residence) Regulations 2008 (opens in new window).
- The Mental Capacity (Deprivation of Liberty, Monitoring and Reporting; and Assessment Regulations 2009 (opens in new window).
- The Mental Capacity (Deprivation of Liberty, Appointment of Relevant Person’s Representative) (amendment) Regulations 2008 (opens in new window).
- The Mental Health Act 1983 (as amended by the MHA 2007) (opens in new window).
- Mental Health Act 1983 Code of Practice (as amended by the MHA 2007) (opens in new window).
- Human Rights Act 1998 (opens in new window).
- The Deprivation of Liberty Safeguards 2008 Code of Practice (opens in new window).
- Data Protection Act 1998 (opens in new window).
- P and Q and Cheshire West (Supreme Court Judgment, laid down on the 19 March 2014) (opens in new window).
12 Appendices
12.1 Appendix A Deciding whether the MHA and, or MCA-DoLS will be available to be used
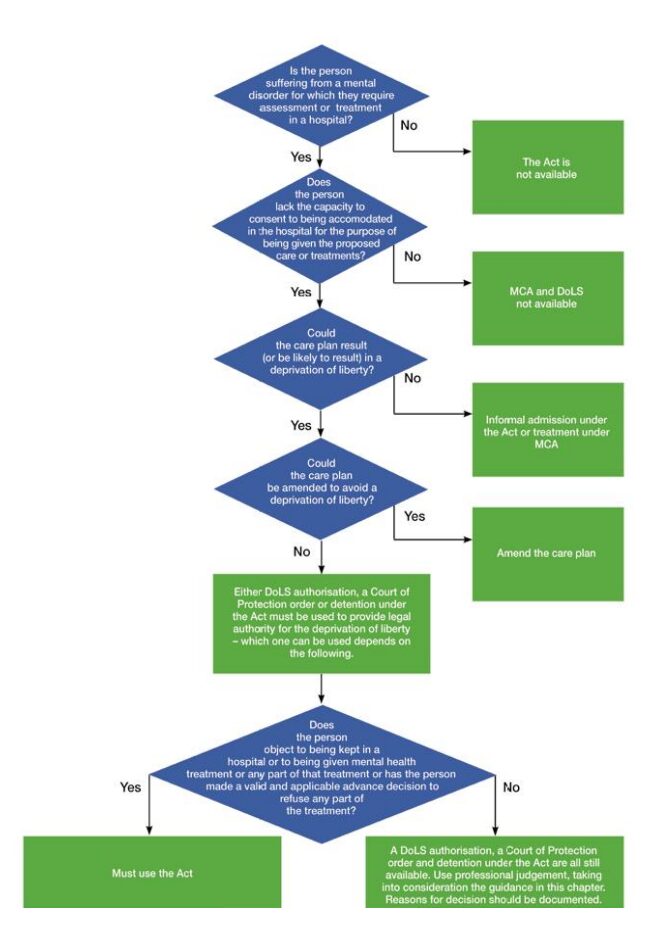
- Is the person suffering from a mental disorder for which they require assessment or treatment in a hospital?
- No, the act is not available.
- Does the person lack the capacity to consent to being accommodated in the hospital for the purpose of being given the proposed care or treatments?
- No, MCA and DoLS not available.
- Could the care plan result or be likely to result in a deprivation of liberty?
- No, informal admission under the act or treatment under MCA.
- Could the care plan be amended to avoid a deprivation of liberty?
- Yes, amend the care plan.
- Either DoLS authorisation, a court of protection order or detention under the act must be used to provide legal authority for the deprivation of liberty, which on can be used depends on the following.
- Does the person object to being kept in a hospital or being given mental health treatment or any part of that treatment or has the person made a valid and applicable advance decision to refuse any part of the treatment?
- Yes, must use the act.
- No, a DoLS authorisation, a court of protection order and detention under the act are all still available. Use professional judgement, taking into consideration the guidance in this chapter. Reasons for decision should be documented.
12.1.1 Appendix A1 DoLS eligibility, interface between DoLS and Mental Health Act 1983 (MHA) guidance
12.1.1.1 Person detained under MHA case A
A person cannot be detained in a hospital under the MHA at the same time as being subject to a DoLS standard authorisation or a Court of Protection order
12.1.1.2 Conditional discharge, case B
If protective conditions are placed on a patient on discharge about where they should reside and the patient lacks the capacity to consent to the conditions, consideration should be given whether the conditions placed on them amount to a DoL. If so it is unlawful to discharge a patient from a detention under the MHA until the DoL is authorised by either the DoLS or the Court of Protection, if in the community. The MHA first tier tribunal must take this into account when making decisions and may need to adjourn the tribunal until the DoL has been authorised. It will be the responsibility of the funding authority to seek authorisation in these cases.
12.1.1.3 Section 17 leave, case B
The responsible clinician (RC) may direct that the patient must remain under the protection of the MHA but may grant section 17 leave to a hospital for treatment of a physical disorder or to a care home for a trial period. If a patient lacks capacity to consent to the placement in a care home and the decision has been made in their best interests a DoLS standard authorisation must be obtained. The RC should ensure that a request for a standard authorisation is made by the registered manger of the care home and that an urgent authorisation is granted if the DoL has not been authorised when the person is admitted to the care home. A DoLS standard authorisation might also be required if leave is granted for treatment of a physical disorder in an acute hospital, particularly if restraint will be needed to provide the treatment. If the person lacks capacity to consent to the admission, care and treatment the RC should liaise with hospital staff in relation to seeking them authorisation.
12.1.1.4 Community treatment orders, case C
Often a residence requirement is not of itself sufficient to amount to a deprivation of liberty. However a continuous package of care and support in the community can amount to a deprivation of liberty if the patient will be subject to continuous supervision and control. If the patient lacks capacity to consent to the care package they will be deprived of their liberty which must be authorised by DoLS if the person is in a care home or the Court of Protection if in a setting other than a care home before the community treatment order is granted. The MHA first tier tribunal must take this into account when making decisions. It will be the responsibility of the funding authority to seek authorisation in these cases.
12.1.1.5 Guardianship, case D
When a person is subject to guardianship under the MHA their guardian can decide where they are to live, but cannot authorise deprivation of liberty and cannot require them to live somewhere where they will be deprived of liberty unless it is authorised. It may be appropriate in some cases where the patient lacks capacity, for a patient to be subject to both guardianship and DoLS (or a declaration of the court). Where the patient is in a care home the case manager should ensure that a request for a standard authorisation is made by the registered manager of the care home and that an urgent authorisation is granted if the DoL has not been authorised when the person is admitted to the care home. If the place the person is required to live is not a care home the case manager should ensure that the funding authority take steps to ensure that the deprivation of liberty is authorised by the Court of Protection.
12.1.1.6 Hospitals only, case E
When considering whether the MHA or DoLS should be used to authorise a deprivation of liberty on an RDASH ward the consultant in charge of the patients care and treatment will need to consider what is in the patient’s best interests and the likelihood of continued compliance and the effect on the regimes’ suitability. They will also consider is the DoLS regime actually available at the time it needs to be used.
12.2 Appendix B Standard operating procedure, deprivation of liberty safeguards (DoLS)
12.2.1.1 Aim of the safeguards
The aim of the deprivation of liberty safeguards (DoLS) is to provide legal protection for those vulnerable people who are, or may become, deprived of their liberty within the meaning of article 5 of the ECHR in a hospital or care home. They do not apply to people detained in hospital under the Mental Health Act 1983 (MHA). They do not provide any power to take and convey people to hospitals or care homes. The safeguards exist to provide a proper legal process and suitable protection in circumstances where deprivation of liberty is unavoidable in a person’s best interests. A DoLS standard authorisation does not in itself authorise care or treatment, only the deprivation of liberty that results from the implementation of the proposed care plan. Any necessary care or treatment should be provided in accordance with the MCA.
12.2.1.2 Roles and responsibilities
12.2.1.2.1 Managing authority
Rotherham Doncaster and South Humber NHS Foundation Trust staff should:
- ensure the DoLS are implemented effectively within the trust by providing systems which support the safeguards and monitoring of compliance
- ensure standard authorisations for deprivation of liberty are sought from the appropriate supervisory body (local authority) in all instances where a person is considered to be deprived of their liberty
- ensure appropriate records are kept
- inform all relevant parties, including the patient, regarding the request for standard authorisation details and detail of the outcome of the request
- ensure the Care Quality Commission (CQC) is notified of the outcome of any requests for standard authorisation
12.2.1.2.2 Appropriate managers
Delegated through the trust’s scheme of delegation to service or team managers, modern matrons, ward managers and registered care home managers.
It is each appropriate manager’s responsibility to ensure their staff are informed of DoLS and receive sufficient training and support to undertake their role. Appropriate managers will also be responsible for ensuring that when a patient is identified as being deprived of their liberty the appropriate documentation is completed and a request for a standard authorisation is submitted to the appropriate supervisory body.
They must also:
- take all steps to minimise the restrictions imposed on a person
- ensure that an urgent authorisation is granted where a deprivation of liberty is apparent
- keep records of any standard authorisation granted
- ensure any conditions placed on a standard authorisation are met
- ensure the DoLS standard authorisation is reviewed, remains current where necessary and is ended when appropriate
- ensure a further standard authorisation is requested (where appropriate) 28 days before a current standard authorisation is due to end
- ensure appropriate advocacy and representation is provided wherever necessary
- ensure the MCA Lead is made aware of all requests for standard authorisation and copied into any further correspondence with the supervisory body
12.2.1.3 Criteria which need to be met
There are six requirements, which each need to be met, for the DoLS to apply. Is the person:
- 18 and over
- suffering from a mental disorder
- lacking capacity for the decision to be accommodated in the hospital or care home
- no decision previously made to refuse treatment or care, or conflict relating to this such as LPA
- not ineligible for DoLS, see guidance in DoL policy
- the person needs to be deprived of liberty, in their best interests
12.2.1.4 Seeking authorisation under DoLS
Whenever it has been identified that a patient who lacks capacity is being, or risks being, deprived of their liberty, and the DoLS criteria is met, the appropriate delegated member of staff, (nurse in charge, following discussion with sister or matron) or registered manager) must apply to the supervisory body (local authority) for authorisation of the deprivation of liberty. The supervisory body will be the local authority for the area in which the person is ordinarily resident. See appendix B1 and B2 for further guidance on DOLS Process and completion of the DoLS Form.
12.2.1.5 Standard authorisation
Staff must request a standard authorisation when it appears likely that, at some time during the next 28 days, someone will be accommodated as an inpatient or a resident in a community home in circumstances that amount to a deprivation of liberty. Where possible this should be done in advance of the person being admitted.
12.2.1.6 Urgent authorisation
Where this is not possible, and staff believe it is necessary to deprive someone of their liberty in their best interests before the standard authorisation process can be completed; staff must issue an urgent authorisation and request a standard authorisation at the same time. An urgent authorisation can be for a maximum of 7 days but may be extended by the supervisory body for up to a further 7 days in exceptional circumstances. Staff will need to consider whether an extension is required on a case by case basis.
12.2.1.7 DoLS forms
The Association of Directors of Social Services (ADASS) has produced standard DoLS forms to be used; however some supervisory bodies have adapted the forms for use locally. Staff should use the DoLS forms within the DoLS questionnaire on SystmOne.
12.2.1.8 Monitoring of the request and standard authorisation
The appropriate delegated member of staff should monitor the progress of the request for standard authorisation, and raise any concerns where deprivation remains unauthorised after the period of the urgent authorisation or where appropriate extension to the urgent authorisation. Once the outcome is received staff should inform the patient and any interested parties of the outcome and where a deprivation of liberty is authorised they should carry out their duties and responsibilities during the period of the standard authorisation as detailed below DoLS process guidance (see appendix B1).
12.2.2 Appendix B1 Guidance on DOLS process
This guidance provides an overview of the process that needs to be undertaken when it is necessary to use the deprivation of liberty safeguards (DoLS) to authorise a deprivation of liberty in a care home or hospital and includes references and guidance on the forms that should be used, who they should be used by, and the timescales required for the completion of actions by all those or everyone involved.
12.2.2.1 Step 1, capacity to consent to admission
Where there is doubt about a patient’s capacity to give informed consent to be admitted to hospital or to reside in a RDASH community home to receive care and treatment, staff involved in admitting the person should on ensure that:
- an assessment of capacity has been undertaken and documented in relation to consent to admission on Form MCA1
And the capacity assessment must focus on the actual regime that will be in place to supervise and control the person. The question is therefore not an abstract one, and the person must have been given the information relevant to the particular care regime that is proposed (or is already in place).
- where the patient lacks capacity to consent to admission a decision is made in their best interest interests and the evidence of this recorded on form MCA2
If the mental capacity assessment and best interests decision has not been made prior to admission this should be undertaken by staff on the ward on the day of admission.
12.2.2.2 Step 2, identifying a deprivation of liberty
Where it is established that the patient lacks the capacity to consent to being admitted to a ward or community home to be being given the care and treatment they require, the assessing clinician must then establish whether the person is being deprived of their liberty. To determine whether a person who lacks capacity is objectively deprived of their liberty, there are two key questions which staff need to ask themselves:
- is the person subject to continuous supervision and control? NB. continuous supervision and control refers to oversight even when the patient is not in the line of sight, it must amount to supervision and have a clear element of control
And:
- is the person free to leave? Note, the person may not be saying this or acting on it, but the issue is about how staff would react if the person did try to leave
12.2.2.3 Step 3, seeking a standard authorisation and granting of urgent authorisation under DoLS
12.2.2.3.1 Request for standard authorisation
Where it is agreed that a person is or will be deprived of their liberty and DoLS is the most appropriate legal framework to treat the patient under, the appropriate delegated member of staff, (nurse in charge, with discussion with sister or matron) or registered manager) must complete a DoLS form 1 request for standard authorisation which can be found via the DoLS folder in the patients record on SystmOne (see appendix B2 on how to complete a DoLS form 1).
12.2.2.3.2 Granting an urgent authorisation
A managing authority can itself give an Urgent Authorisation for deprivation of liberty where either:
- it is required to make a request to the supervisory body for a standard authorisation, but believes that the need for the person to be deprived of their liberty is so urgent that deprivation needs to begin before the request is made
- it has made a request for a standard authorisation but believes that the need for a person to be deprived of liberty has now become so urgent that deprivation of liberty needs to begin before the request is dealt with by the supervisory body
Urgent authorisations should normally only be used in response to sudden unforeseen needs. An urgent authorisation should not be used in circumstances where a person who lacks capacity and is being deprived of their liberty is detained under the MHA and it is proposed that they are removed from the relevant section of the MHA and authorisation under the DoLS is being sought.
Where the patient has already been admitted and is being deprived of their liberty and the MHA does not apply, staff should ensure that they complete the urgent authorisation part of the DoLS form 1 to grant an urgent authorisation for up to 7 days to ensure that the patient is not unlawfully deprived of their liberty until the DoLS assessment can be undertaken.
The urgent authorisation should be granted and the request for a standard authorisation must be made within 24 hours of admission.
The form 1 together with copies of the MCA1 and MCA2 relating to the decision about admission to the ward or care home should be sent by email to the supervisory body (local authority DoLS team) where the patient was residing prior to admission.
Email addresses for the LA teams in the 3 localities of the trust are:
- Doncaster: dols@doncaster.gov.uk
- Rotherham: dols@rotherham.gov.uk
- North Lincolnshire: dols@northlincs.gov.uk
For contact details of local authorities outside the three trust localities contact the trust MCA lead.
If the form 1 has been completed by nursing staff the ward manager or modern matron should be copied into the email. This ensures replies are not just sent to nursing staff who may be on leave etc. and avoids delays in requests for further information and outcomes of requests.
The trust MCA lead should also be copied into all emails regarding requests for authorisation requests and any further correspondence with the supervisory body in order that a central record of the request can be maintained, and up-to-date statistics can be provided to relevant committees of the trust.
12.2.2.4 Step 4, storing of DoLS information
Staff should record all requests on the patients record via the DoLS questionnaire. Information regarding the request should be recorded on the DoLS status and updated during the process.
Copies of any emails and the completed DoLS form 1 should be kept on the person’s case file or scanned onto the appropriate patient electronic record.
12.2.2.5 Step 5, notification
As soon as practical and appropriate to do so the patient must be informed that an application for a standard authorisation has been made and be given a copy of the trusts DoLS Easy read leaflet, see appendix B3. This can be found in the DoLS questionnaire in the patients record. A record of the date and time the patient was notified of request should be entered on the DoLS status.
As far as possible and appropriate the patient’s family, and any friends, carers involved in the persons care should also be informed that a request has been made.
12.2.2.6 Step 6, request for extension to the urgent authorisation
If there are exceptional reasons why the request for a standard authorisation cannot be dealt with within the period of the urgent authorisation (for example, within 7 days), the delegated staff member should ask the supervisory body to extend the duration of the urgent authorisation or a further 7 days, by completing the request for an extension to the urgent authorisation section on DoLS Form 1 or form 1A (Doncaster) and resubmitting to the supervisory body.
Details of the request should be entered on the DoLS status in the patients record.
The code of practice gives an example of when an extension may be justified as an assessor not being able to make contact with someone who it is essential to speak to. The supervisory body must decide what it considers to be “exceptional reasons”.
The code is very clear about the following:
- a decision about exceptional reasons must be soundly based and defensible
- it would not usually be justified due to staff shortages
- an urgent authorisation can only be extended once
Due to the unprecedented numbers of applications following the Supreme Court judgment it is likely that there will be delays in the requests being processed. Staff should, at this point in time consider these as exceptional circumstances and request an extension to the urgent authorisation at the same time the request for a standard authorisation is made.
If an authorisation has not been received after the period of extension the deprivation of liberty will be unauthorised. It is the responsibility of the person who made the request to contact the supervisory body periodically to check on the process of the request and to update the MCA lead on the status of the authorisation.
12.2.2.7 Step 7, cancellation of request before outcome of request for authorisation received
If there are any changes to the patient’s condition or care arrangements, (for example, detention under the MHA, the patient regains capacity, is transferred to another setting, or is discharged home), before the outcome of the request for authorisation is received staff must inform the supervisory body by email of the changes immediately and ask for the request to be withdrawn.
The MCA lead should be copied into any correspondence with the supervisory body.
The DoLS status should be updated.
If there has been a change in the person capacity to consent to being a patient on a ward or resident in a community home a mental capacity assessment should be carried out and recorded on MCA1. A copy of the assessment should be sent to the supervisory body with the notification of change of circumstances.
If the patient has been discharged from a ward or transferred to another care setting or hospital from a community home, details of when and where they were discharged should be included in the notification.
The supervisory body should return DoLS form 6, authorisation not granted.
This form will be issued when some all or no assessments have been completed, but the person dies or is discharged therefore the full authorisation process cannot be concluded as there will be no authority to proceed.
Due to the backlog many supervisory bodies have experienced in processing their applications since 2014 it may be the case that by the time an application can be processed it is no longer actually needed. These applications will be classed as authorisation not granted.
Receipt of the DoLS form 6 should be recorded in the patients record on the DoLS status. A copy should be sent to the MCA lead.
Staff at the receiving hospital or new care placement should be made aware that the patient was subject to a DoLS standard authorisation, prior to the transfer and where possible a standard authorisation sought by the new managing authority from the relevant supervisory body.
12.2.2.8 Step 8, the assessment process
The supervisory body should acknowledge receipt of the request for a standard authorisation and prioritise the case in line with ADASS guidance.
Requests in relation to patients in hospital should be treated as (red) high priority; however, this will depend on the availability of assessors within the supervisory body.
The supervisory body will allocate a best interest assessor (BIA) and a mental health assessor (MHA) to undertake assessments. The assessors should contact the ward or registered manager to make arrangements to visit the patient and to consult with staff involved in the patient’s care.
Details of the assessors and dates of the assessment was carried out should be recorded in the patients record on the DoLS status.
12.2.2.8.1 Independent mental capacity advocate (IMCA)
In circumstances where the patient has no one to represent them (for example, no family, friends, carers) the supervisory body will appoint a (39A) independent mental capacity assessor (IMCA) to support the patient through the assessment process.
Details of the advocate and the dates of any visits should be recorded in the patient’s record on the DoLS status.
Both assessors and any IMCA will be required to sign the visitor’s book when visiting the patient or make an entry in the patient’s case.
Both assessors and the IMCA may examine and take copies of any health record or record held by a community home or on a ward relating to the deprivation of liberty which they consider relevant to their assessment.
12.2.2.8.2 Conditions placed on the authorisation
If the BIA is considering making the standard authorisation subject to conditions these must be discussed with staff from the managing authority before the BIA completes their assessment. A record of any discussion with the BIA must be entered in the patients record and the DoLS status updated.
As it may be sometime before the copy of the standard authorisation is received staff should work towards meeting any suggested conditions as soon as possible.
12.2.2.9 Step 9, outcome of assessment, standard authorisation not granted
If during the assessment process it is clear that the all the requirements are not met. The supervisory body will issue a DoLS form 6.
The supervisory body will state why it is prohibited from giving a standard authorisation in relation to the named patient and will detail which requirements were not met.
Not all assessments will be completed because when a person fails one requirement, a standard authorisation may not be granted and all other ongoing assessments must stop.
Due to the large number of applications following the Supreme Court judgement, many supervisory bodies are finding that a person may have died or been discharged before any or all assessments are carried out. Therefore, it is not possible to grant a standard authorisation as the person is no longer in the setting. In this case the supervisory body will note which assessments were not carried out and why.
On receipt of the standard authorisation not granted DoLS form 6 the delegated staff member should record the outcome of the request in the patients record and update the DoLS status.
The MCA lead should be informed of the outcome.
12.2.2.10 Step 9, outcome of assessment, standard authorisation granted DOL authorised
Where all the assessments in the authorisation process indicate that the patient meets all the qualifying criteria, the DoLS standard authorisation DoLS form 5 will be issued by the supervisory body, together with copies of the BIA assessments DoLS form 3 and MHA assessments DoLS form 4 and any IMCA report.
On receipt of the standard authorisation DoLS form 5 and copies of assessments the delegated staff member should check the patient’s details entered on the standard authorisation and information contained within the assessments are correct and record the details of the period of the standard authorisation and any conditions it is subject to in the patients record and the DoLS status updated.
The supervisory body should be notified of any discrepancies immediately.
Hard copies of any reports received should be scanned onto the relevant patient record and the DoLS status updated. The MDT should be made aware that the patient is subject to a DoLS standard authorisation.
The date the standard authorisation is due to expire should be recorded on the patients record and the DoLS status updated. A reminder 28 days prior to the date of expiry should be put into the ward or home diary and where possible the Outlook calendar of the ward or care home manager. This will act as a reminder to request a further standard authorisation if required.
The MCA DoLS lead will also send a reminder 28 days before the authorisation is due to expire.
12.2.2.10.1 Notification of the standard authorisation
The trust has a duty to ensure that the patient (where practically possible) is made aware of the effect of the standard authorisation (Dols form 5) and provided with a copy of it and all other assessments.
The supervisory body may provide a hard copy for the patient however until it is received staff must ensure that the patient is aware of their rights to request a review of the standard authorisation, and their right to challenge the standard authorisation in the Court of Protection, under section 21A of the act. All patients under a standard authorisation should be given a copy of the trusts DoLS rights leaflet (appendix B5).
The date and time the patient was notified of the standard authorisation and their rights should be entered in the patients record and the DoLS Status updated.
12.2.2.10.2 Conditions
If the standard authorisation is subject to any conditions the multi-disciplinary team will need to discuss how the conditions can be met, agree actions and ensure that the actions are carried out as soon as possible. If the conditions cannot be met the supervisory body must be informed as soon as possible giving the reasons why they cannot be met as this can affect the legality of the standard authorisation.
12.2.2.10.3 Recommendations
During the assessment process BIAs often become aware of deficits in the care planning process which need to be addressed but are not legitimate conditions.
On receipt of the standard authorisation DoLS form 5 staff should check to see if any recommendations have been suggested.
Where recommendations have been made actions should be agreed and carried out as soon as possible to ensure the concerns are addressed.
12.2.2.10.3 Care Quality Commission (CQC)
The trust has a duty to notify the CQC of the outcome of any requests for a standard authorisation. For inpatient services this will be completed by the trust MCA lead. It is important therefore to ensure the MCA lead is advised of the outcome. For residents in RDaSH community homes this will be completed by the registered manager.
12.2.2.11 Step 10, during the period of the standard authorisation
12.2.2.11.1 Relevant persons representative (RPR)
Once a standard authorisation is granted the supervisory body must appoint a RPR.
Details of the RPR can be found at the end of the standard authorisation on DoLS form 5. This information should be recorded on the patients record and the DoLS status updated.
It is important that the RPR has sufficient contact with the patient to ensure that their best interests are being safeguarded. In order to fulfil their role, therefore, the RPR will need to be able to have face-to-face contact with the relevant person.
A record should be maintained of any visits or requests for information made by the RPR on the DoLS record during the period of the standard authorisation.
If the RPR does not maintain contact with the person, the rights of the patient may not be sufficiently protected. This should be at least every 2 weeks.
If the RPR does not maintain contact with the patient the supervisory body should be informed.
It is important that the RPR is consulted about any proposed changes to the patient’s care plan.
12.2.2.11.2 Independent mental capacity advocate (IMCA)
The DoLS allows for the appointment of a (39D) IMCA to support the patient during the period of the standard authorisation. If it is felt that the person would benefit from this support staff should contact the supervisory body to request that an IMCA be appointed.
12.2.2.11.3 Objection to placement
If a member of staff believes that a patient, who is subject to a standard authorisation, in a community home is objecting to the placement or is showing signs that they are unhappy with the placement. They should contact the persons RPR to ask them to identify whether P wishes or should be supported to challenge the authorisation. If a person, who is subject to a standard authorisation on one of the trusts’ hospital wards then objects to being held on the ward, staff should consider the use of the MHA to authorise the detention
12.2.2.12 Step 11, suspension of a standard authorisation
Regulations allow for a standard authorisation which is currently in force to be suspended only when the person is no longer eligible for DoLS because of a conflict with the MHA.
If a person under a standard authorisation, then is detained in a hospital under the MHA the authorisation can be suspended for up to 28 days in which case staff should complete DoLS form 7 and send to the supervisory body.
Details of the notification of suspension should be entered on the patients record and the DoLS status updated. A date should be put in the ward diary to notify the supervisory body of the end of the suspension.
The MCA lead should be copied into any correspondence with the supervisory body.
If the person returns during the 28 day or does not return after the time period has lapsed the relevant member of staff should complete the second part of the DoLS form 7 and send to the supervisory body to inform them whether of the situation. If the patient has returned the standard authorisation is once again in force. If the patient has not returned or is still detained under the MHA within this time period, the authorisation will cease to be in force and the supervisory body will issue a DoLS form 9.
12.2.2.12.1 Transfer to acute care
If the person who is subject to a standard authorisation is admitted to an acute hospital on physical ill health grounds for a short period or another temporary setting or is temporarily absent for another reason. There is no requirement to request suspension.
There is currently no form to cover this scenario. However, the most pragmatic approach (as advised by ADASS) seems to be as follows:
- if the new setting requests a standard authorisation, then the existing one is automatically ended and so no action is needed other than to inform the supervisory body of the transfer
- alternatively, if the absence is likely to be short and no DoLS. authorisation is requested by the new setting, again, do nothing. This will leave the standard authorisation in place for when the person returns
- if the absence is likely to be for a long period, or there is a likelihood the patient will not return to your setting, use the relevant section in DoLS form 10, request for review to inform the supervisory body so the DoLS authorisation can be formerly ended
The MCA Lead should be copied into any correspondence with the supervisory body.
Where a standard authorisation ceases to be in force the supervisory body will issue a DoLS form 9. On receipt of the DoLS form 9 the relevant member of staff should enter the details in the patients record and the DoLS status updated.
The MCA lead should be informed of the date the standard authorisation ceased.
12.2.2.13 Step 12, changes during period of standard authorisation, request for review
12.2.2.13.1 Care and treatment plan
If there are any significant changes to the patient’s condition or care arrangements, during the period of the standard authorisation staff must inform the supervisory body immediately by completing DoLS Form 10.
Any decision regarding changes which result in the care and treatment being more restrictive or the use of covert medication not identified on the authorisation will need to be made under the provisions of the MCA in the person best interests. The RPR should be involved in these decisions.
Where a best interests decision is made, a review of whether the DoL is still in the persons’ best interest should be requested on DoLS form 10 and sent to the supervisory body with the MCA1 and MCA2.
The MCA lead should be copied into any correspondence with the supervisory body.
After the review has taken place the supervisory body will return the DoLS form 10 with the supervisory body’s decision section completed.
If the qualifying requirements are still met the standard authorisation will remain in force.
Where a standard authorisation ceases to be in force the supervisory body will issue a DoLS form 9.
On receipt of the outcome or DoLS form 9 the relevant member of staff should enter the details in the patients record and the DoLS status updated.
The MCA lead should be informed of the date the standard authorisation ceased.
12.2.2.13.2 Capacity
If there has been a change in the person capacity to consent to being a patient on a ward or resident in a community home a mental capacity assessment should be carried out and recorded on MCA1. A copy of the assessment should be sent to the supervisory body with the request for a review DoLS form 10.
After the review has taken place the supervisory body will return the DoLS form 10 with the supervisory body’s decision section completed.
If the qualifying requirements are still met the standard authorisation will remain in force.
Where an authorisation ceases to be in force the supervisory body will issue a DoLS form 9.
On receipt of DoLS form 9 the relevant member of staff should enter the details in the patients record and the DoLS status updated.
The MCA lead should be informed of the date the standard authorisation ceased.
12.2.2.13.3 Patient discharged
If the patient has been discharged from a ward or transferred to another care setting or hospital from a community home, details of when and where they were discharged should be included on the DoLS form 10. The section “review to cease the DoLS standard authorisation” should provide details of why a standard authorisation is no longer needed, this should include date of discharge and where the person was discharged to.
If the person lacks capacity to consent to discharge plans which involve a change of residence or admission to another hospital copies of the assessment of capacity MCA1 and best interests decision record MCA2 to support the decision should be provided to the supervisory body with the DoLS form 10.
Where a standard authorisation ceases to be in force the supervisory body will issue a DoLS form 9.
On receipt of the DoLS form 9 the relevant member of staff should enter the details in the patients record and the DoLS status updated.
The MCA lead should be informed of the date the standard authorisation ceased.
Staff at the receiving hospital or new care placement should be made aware that the patient was subject to a DoLS standard authorisation, prior to the transfer and where possible a standard authorisation sought by the new managing authority from the relevant supervisory body.
12.2.2.13.4 Death under detention
From 3 April 2017, deaths of people subject to the deprivation of liberty safeguards (DoLS) no longer trigger a mandatory coroner’s inquest, although as with any death consideration must still be given in each case to whether any of the other grounds for reporting the death may apply, including if the death was unexpected, unnatural or if the family have issues about the care.
As soon as possible after the death staff should complete a DoLS form 12 A password protected copy should be sent to the supervisory body (the MCA lead should be copied into the email).
An IR1 form should also be completed in line with the trusts incident management policy.
Where a standard authorisation ceases to be in force due to the person death the supervisory body will issue a DoLS form 9.
On receipt of the DoLS form 9 the relevant member of staff should enter the details in the patients record on the DoLS status.
The MCA lead should be informed of the date the standard authorisation ceased.
12.2.2.14 Step 13, expiry of standard authorisation
When an existing DoLS standard authorisation is coming to an end staff will need to consider whether a further standard authorisation will be required. It is possible, at any stage, that things have changed, and the person no longer needs such a restrictive environment or the person now has capacity to consent to the arrangements.
In this case DoLS form 10 should be completed by the relevant member of staff and sent to the supervisory body.
In circumstances where a further standard authorisation is required, staff will need to complete a DoLS form 2 request for further standard authorisation. This should be requested 28 days before the expiry date. Any delays may result in the patient being unlawfully detained.
The amount of information needed when a further request for new standard authorisation is much less than the initial requirement as the supervisory body will have already received a great deal of personal details and comprehensive information about the patient and will have carried out the necessary assessments to grant an initial standard authorisation.
The DoLS form 2 will need to include up-to-date information and any changes to the care and treatment plan and the restrictions in place and should not be a copy of the original request. If the previous standard authorisation was subject to conditions the new request should include information about how the conditions have been met.
Once completed the DoLs form 2 should be password protected and sent to the supervisory body as detailed in step 3.
Details of the request should be recorded on the DoLS record and the patient notified as detailed in step 5.
12.2.3 Appendix B2 Guidance on completion of DoLS form 1 request for standard authorisation
The DoLS form 1 has to be accurate, complete and comprehensive to facilitate the process and enable the assessors to have some insight into the person’s circumstances before they commence their assessments. All questions must be answered or explanation given as to why the information has not been provided.
12.2.3.1 Page 1, this page will take you through the patient’s basic details
It is helpful to assessors if you can summarise the patients’ relevant medical history. If you know this, you should include details of the patients mental disorder, current conditions and symptoms.
It is important to inform the supervisory body of any sensory or communication problems in order that assessors and advocates can prepare for visits, to ensure all practicable steps are taken to enable the patient to participate in the assessment. This is in accordance with requirements of the accessible information standard.
The Doncaster forms allow you to choose from dropdown lists.
12.2.3.2 Page 2, date from which the SA is required
An urgent authorisation can only be granted for 7 days, unless an extension of the urgent authorisation is granted by the supervisory body. Therefore the date the standard authorisation is required, is the 8th day after the request is signed as the urgent authorisation will cease at midnight on the 7th day.
Doncaster forms do not require a date at this point you just have to choose yes or no. The date the SA is required is after relevant medical history.
12.2.3.3 Pages 2 or 3, purpose of the urgent or standard authorisation, this provides two essential pieces of information
Firstly a description of the care and treatment, in other words, why does the patient need to be accommodated in the hospital or care home?
It is important to say why and when the patient was admitted but should focus on what is happening now rather than pre-admission. If the person has previously been detained under the MHA it is important to say when and why this was rescinded.
It asks for a detailed description of the care and, or treatment the patient is receiving whilst on the ward or in the care home. It should not include vague statements such as “24 hour care”.
It should include details of personal care and support, supervision, help with mobility, medication, support with behavioural issues, types of choice the patient has and any medical treatment they receive. If in a care home it may include additional support should have help with finances, support with social activities or maintaining relationships etc.
Remember the person’s ability to consent to medication should be considered and where there is doubt about the person ability to consent a mental capacity assessment should be undertaken and recorded on MCA1. Where the person lacks capacity any decisions relating to the prescribing and administering of medication should be made in the patient’s best interests and recorded on MCA2. Copies of the MCA paperwork should be available for the BIA Assessor to consider as part of their assessment.
Any details of use of covert medication being given in the person best interest should include details of the management plan in relation to the medication being prescribed.
12.2.3.3.1 Remember if it is not listed you are not authorised to give it
If it is impractical to attach a full care plan it must be available for assessors and any independent mental capacity advocate (IMCA) when they visit.
12.2.3.3.2 Secondly evidence of why the patient meets the acid test for a deprivation of liberty
In other words, what restrictions and restraints is the patient subject to?
This section should provide a description of all the measures that are in place which have led to a request for a standard authorisation:
- describe the environment the person is in
- whether it is a temporary or permanent arrangement
- if a care home who has determined that they live there
- why the person is subject to, continuous supervision and control and not free to leave
Staff must describe the nature of any restrictions in place and the degree and intensity in which they are applied.
This should include any forms of restraint which are being used to keep the person safe and the type, manner which it is applied, the frequency and duration and the effect on the patient.
For example it is better to say: “Mrs X has to be reassured and redirected by staff at least 4 to 5 times a day as she is distressed and wants to leave the ward.” Rather than, “Mrs X says she wants to leave.”.
It is better to say: “1-to-1 support is in place at all times of day, when John is in his room or moving around the building, when he has meals or takes part in social events. However at night there is less support as there is a sleeping night and no checks are made beyond the routine checks.” Rather than, “John has 1-to-1 support.”.
Staff should also say why the necessary care and treatment cannot be provided in a less restrictive way and what if any alternatives to a deprivation of liberty have been tried or considered and what harm the patient is likely to come to if they are not deprived of their liberty.
12.2.3.3.3 Examples of restrictions and restraint on an adult mental health ward
- Blanket restrictions. These include, limited access to bedrooms during the day; restrictions on access to parts of the ward such as kitchen areas; restrictions to avoid risks such as falls
- Setting of observation and monitoring levels.
- Requirements for patients to be escorted in certain parts of the ward or site.
- The physical environment (for example, wards not on ground level) may limit patients’ access to the outdoors.
- The prescription and administration of medication to a patient who lacks capacity to consent to it, in particular medication to sedate and, or to control behaviour that challenges us.
- The extent to which the patient is required to adhere to a timetable.
- Locked doors, or use of “baffle locks”, unless patients have the code and are able to come and go as they please.
- The concept of “protected time” is a valuable means of ensuring that patients have quiet periods during the day but also represents control over the activities of patients.
- Limited visiting time.
- Lack of easy access to TV, phones, internet.
- Sanctions, such as time out, for behaviour that challenges us.
- Restriction of access to finances.
- Seclusion (often described in misleading terms, not recognised as such and thus not reviewed in accordance with the Code of Practice to the MHA 1983).
- The need for restraint and other physical interventions, in the patient’s best interests, to control behaviour, especially where such restraint is regular.
- Assuming control over what the individual does with their time.
12.2.3.3.4 Additional examples of potentially liberty restricting-measures that may be found in a DCIS hospital ward (Hazel)
- The need for restraint and other physical interventions, in the patient’s best interests, to, deliver personal care.
- Mittens, or forms of restraint used to prevent a patient removing or interfering with a nasogastric feeding tube.
- Raised bedrails or other restrictive equipment.
- Catheter bag attached to bed.
- A patient being placed in a chair and being unable to move from the chair without assistance.
- Frequency and intensity of observation and monitoring levels.
- The requirement for a patient to remain in a certain area of the ward.
- The requirement that a patient does not leave the ward, accompanied by a plan that, if he does, he will be returned to the ward.
12.2.3.3.5 Additional examples of potentially liberty restricting-measures that may be found in a hospice setting include
- That the circumstances are no longer covered by a consent given on admission.
- Administering sedatives to decrease anxiety and agitation.
- Chemical restraint.
- Constant supervision in case of terminal agitation.
- Restricting movement of patients who are mobile, so that they are not free to leave the hospice grounds because they may be a danger to themselves.
12.2.3.3.6 Questions for front-line practitioners working on inpatient wards
These questions may help establish whether an individual is deprived of their liberty in this context:
- what liberty-restricting measures are being taken?
- when are they required?
- for what period will they endure?
- what are the effects of any restraint or restrictions?
- how are any restraints or restrictions applied?
- are there less restrictive options available?
- is force or restraint (including sedation) being used to admit the patient to a hospital to which the person is resisting admission?
- is force being used to prevent a patient leaving the hospital, hospice, or care home where the person is persistently trying to leave?
- is the patient prevented from leaving by distraction locked doors, restraint, or because they are led to believe that they would be prevented from leaving if they tried?
- is access to the patient by relatives or carers being severely restricted?
- is the decision to admit the patient being opposed by relatives or carers who live with the patient?
- has a relative or carer asked for the person to be discharged to their care and is the request opposed or has it been denied?
- are the patient’s movements restricted within the care setting?
- are family, friends or carers, prevented from moving the patient to another care setting or prevented from taking them out at all?
- is the patient prevented from going outside the hospital or hospice (escorted or otherwise)?
- is the patient’s behaviour and movements being controlled through the regular use of medication or equipment?
- do staff exercise complete control over the care and movement of the person for a significant period?
- is the patient constantly monitored and observed throughout the day and night?
12.2.3.3.7 In addition to the measures described in above the following additional features may be present in community care homes for adults with learning disabilities
- A perimeter fence with a locked gate.
- Keypads on doors which residents cannot unlock.
- A structured routine.
- Monitoring and observation.
- Use of medication, including PRN.
- Use of physical interventions of any type in response behaviour that challenges us.
- Use of sanctions such as “time out”.
- Residents being told to spend time in a “quiet room” as part of de-escalation.
- A care plan which provides that a resident must be escorted outside the care home(including where this results from physical needs, for example, a resident who needs someone to push their wheelchair).
- Restrictions on developing sexual relations.
- Mechanical restraints, for example, lap straps.
- Decisions about contact with friends and family taken by others.
12.2.3.3.8 Questions for front line staff working in community care homes
These questions may help establish whether an individual is deprived of their liberty in this context:
- are any of the liberty-restricting measures described above applied to the resident concerned? If so which and for what reason?
- are there any restrictions on the person’s contact with others? If so do they restrict contact beyond the home’s usual visiting arrangements?
- is the person’s access to the community restricted in any way? For example must they be escorted? What would staff do if they left the home alone or sought to do so?
- is the person required to be at the care home at specified times?
- must the person be escorted either within or outside the care home?
- is the person required to say where they are going when leaving the care home?
- is the person required to take part in a programme of treatment? What happens if they do not?
- is the person required to take medication? What are the arrangements for this? What happens if they do not take it?
- is the person required to remain abstinent from alcohol or drugs?
- are there drugs tests?
- is any legal framework currently being used, for example, conditional discharge, CTO or guardianship? If so, what are the precise terms?
- is the person required to observe an exclusion zone? If so how large is it and what implications does it have? For example, visits to family members?
- is the person required to avoid specific settings?
- are decisions about contact with friends and family taken by others?
- is choice extremely limited even in terms of everyday activities?
- is restraint used to deliver personal care?
- are the person’s wishes often overridden, in their best interests
- could any of the liberty-restricting measures be dispensed with?
12.2.3.4 Information about interested parties and others to consult
The BIA has a duty to consult all interested parties as part of the process. It is important that you provide sufficient contact details.
An interested person is any of the following:
- the patients spouse or civil partner
- where the patient and another person of the opposite sex are not married to each other but are living together as husband and wife, the other person
- where the patient and another person of the same sex are not civil partners of each other but are living together as if they were civil partners, the other person
- the patient’s children and stepchildren
- the patient’s parents and stepparents
- the patients brothers, sisters, half-brothers, half-sisters, stepbrothers and stepsisters
- the patient’s grandparents or grandchildren
The form also asks for other people such as anyone caring for the patient or interested in their welfare. This should include any professional staff involved in the persons care, such as consultants, social workers, occupational therapist, CPN, CMH nurse, care staff etc. If there is insufficient space in the boxes provided the person name, contact details and relationship to the patient should be included in – Other relevant information.
12.2.3.5 Any donee of a registered lasting power of attorney for health and welfare granted by the person (LPA)
If a registered LPA is in place for health and welfare a copy should be taken and kept in the patients’ case notes. Staff should include the date the LPA was registered with the office of the public guardian in, other relevant information and identify whether there is any restriction on the attorney.
12.2.3.6 Any deputy for health and welfare appointed for the person by the court of protection
If a court appointed deputy is in place for health and welfare a copy of the court order should be taken and kept in the persons’ case notes. Staff should include the date the order in, other relevant information and identify any limitations on the deputy’s decision-making power.
12.2.3.7 Whether it is necessary for a 39A independent mental capacity advocate (IMCA) to be instructed
The supervisory body has a duty to instruct an IMCA if the person has no one appropriate to consult in relation to the DoL. Staff need to ensure the correct box is ticked so as an IMCA can be appointed if required.
12.2.3.8 Whether the patient has an advance decision to refuse treatment (ADRT)
Checks should be made to ascertain whether the patient has made an ADRT and tick the appropriate box.
If the ADRT is valid and applicable to some or all of the treatment that is the purpose for which the authorisation is requested. The standard authorisation cannot be given. If staff are aware of any ADRT and are unsure if it is valid and applicable they should contact the trust MCA lead for advice.
12.2.3.9 Mental Health Act 1983 (MHA)
If the patient is subject to some aspect of the MHA, for example in a care home under a guardianship order, staff need to provide details of the order including the date the person became subject to the order, the date it is due to expire and any conditions it is subject to.
12.2.3.10 Other relevant information
This section should be used to provide any other relevant information that you haven’t included elsewhere, including any current safeguarding investigations which are taking place.
12.2.3.11 Signing and dating the form
The responsible staff member should type their name in the signature box. The supervisory body may accept this as a signature providing the date and time are the same as the date it is sent to the supervisory body by email. If the patient is currently being deprived of their liberty it should be the same date the urgent authorisation is issued.
Once the form has been signed and dated staff should confirm by typing in their name to say, the patient and any interested parties have been notified of the request for a standard authorisation.
12.2.3.12 Important data collection
This information is required for the quarterly DoLS returns to the Health and Social Care Information Centre which the supervisory body are required to submit. It is important that this information is provided. Doncaster forms allow you to choose from a drop-down box.
12.2.3.13 Urgent authorisation
Wherever possible, the application for a standard authorisation should be made before the DoL is occurring. However where a DoL needs to commence before a standard authorisation can be obtained, this section of the form should be completed and signed.
The tick boxes are straightforward as all of the details will have been provided earlier in the form.
The urgent authorisation can be given for a period of up to seven calendar days and comes into force at the time it is signed.
The urgent authorisation will expire at midnight on the seventh day of issue. This includes the date of signing. For example an urgent authorisation issued on the first will end on the seventh and a standard authorisation will be needed from the eighth day.
Although the original intention was that an urgent authorisation would be for “sudden unforeseen needs” in practice this has not been the case as DoLS assessments are not being completed within the statutory timescales due to influx of requests for authorisations being received by supervisory bodies.
12.2.3.14 Request for an extension to the urgent authorisation
The intention of adding the request for an extension of an urgent authorisation to the initial form is to identify whether this will be required at the beginning of the process due to the unprecedented numbers of applications following the Supreme Court judgment as it is likely that there will be delays in the request being processed.
Staff should, at this point in time consider these exceptional circumstances and complete the request for the extension at the same time the request for standard authorisation is made. The supervisor body should when acknowledging receipt of the request for the standard authorisation confirm that the period of the urgent authorisation has been granted for up to a further 7 days and amend the end date.
Doncaster has created a separate form 1A for this purpose.
12.2.4 Appendix B3 Deprivation of liberty safeguards easy read leaflet
12.2.5 Appendix B4 Deprivation of liberty safeguards, process flowcharts
12.2.5.1 Seeking an authorisation under the deprivation of liberty safeguards
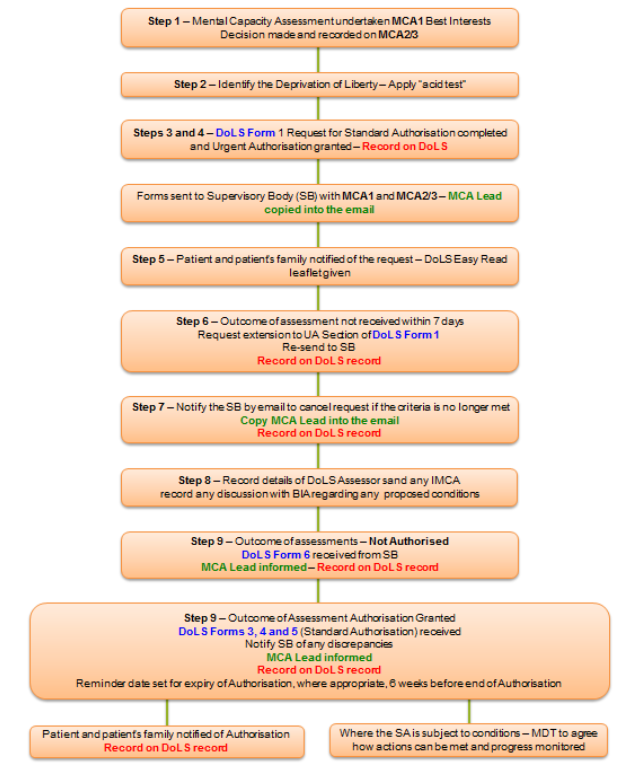
- Mental capacity assessment undertaken MCA1 best interests decision made and recorded on MCA2/3.
- Identify the deprivation of liberty, apply acid test.
- DoLS form 1 request for standard authorisation completed and urgent authorisation granted, record on DoLS.
- Forms sent to supervisory body (SB) with MCA1 and MCA2/3, MCA lead copied into email.
- Patient and patient’s family notified of the request, DoLS easy read leaflet given.
- Outcome of assessment not received within 7 days, request extension to UA section of DoLS form, re-send to SB, record on DoLS record.
- Notify the SB by email to cancel request if the criteria is no longer met, copy MCA lead into email, record on DoLS record.
- Record details of DoLS assessors and any IMCA record any discussion with BIA regarding any proposed conditions.
- Outcome of assessment, not authorised, DoLS form 6 received from SB, MCA lead informed, record on DoLS record.
- Outcome of assessment authorisation granted, DoLS forms 3, 4, and 5 (standard authorisation) received, notify SB of any discrepancies, MCA lead informed, record on DoLS record. Reminder date set for expiry authorisation, where appropriate, 6 weeks before end of authorisation:
- patient and patient’s family notified of authorisation, record on DoLS record
- where the SA is subject to condition, MDT to agree how actions can be met and progress monitored
12.2.5.2 During the period of authorisation, trust responsibilities
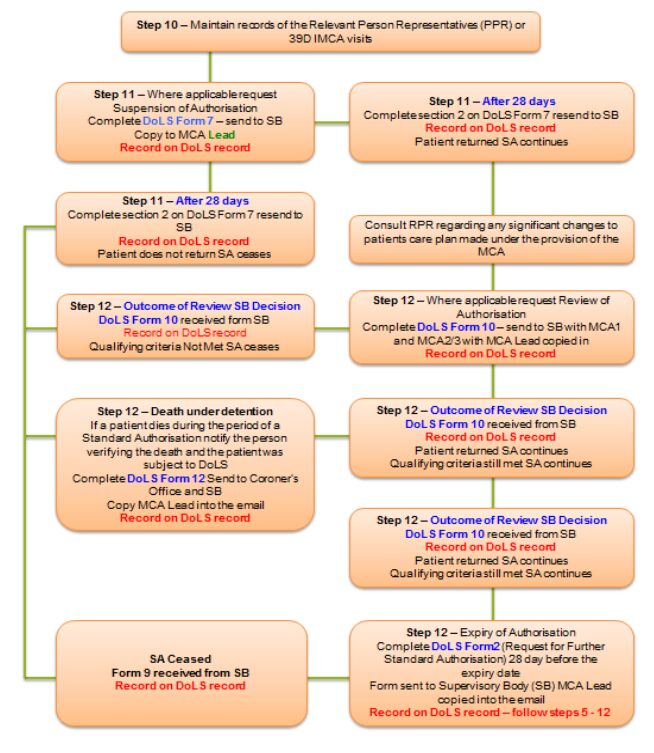
- Maintain records of the relevant person representatives (PPR) or 39D IMCA visits.
- Where applicable request suspension of authorisation, complete DoLS form 7, send to SB, copy to MCA lead, record on DoLS record:
- after 28 days, complete section 2 on DoLS form 7 and resend to SB, record on DoLS record, patient does not return SA ceases
- after 28 days, complete section on DoLS form 8 and resend to SB, record on DoLS record, patient returned SA continues
- consult RPR regarding any significant changes to patients care plan made under the provision of the MCA
- Outcome of review SB decision DoLS form 10 received form SB, record on DoLS record, qualifying criteria not met SA ceases:
- where applicable request review of authorisation, complete DoLS form 10, send to SB with MCA1 and MCA2/3 with MCA lead copied in, record on DoLS
- death under detention, if a patient dies during the period of standard authorisation notify the person verifying the death and the patient was subject to DoLS, complete DoLS form 12 send to coroner’s office and SB, copy MCA lead into email, record on DoLS record
- outcome of review SB decision, DoLS form 10 received from SB, record on DoLS record, patient returned SA continues, qualifying certain still met SA continues
- expiry of authorisation, complete DoLS form 2 (request for further standard authorisation) 28 day before the expiry date, form sent to supervisory body (SB) MCA lead copied into email, record on DoLS record, follow steps 5 to 12
- SA ceased, form 9 received form SB, record on DoLS record.
12.2.6 Appendix B5 The deprivation of liberty safeguards (DoLS) standard authorisation, your rights letter
Document control
- Version: 7.
- Unique reference number: 80.
- Approved by: Mental health legislation operational group.
- Date approved: 12 January 2023.
- Name of originator or author: Mental capacity act lead.
- Name of responsible individual: Mental health legislation operational group.
- Date issued: 31 January 2023.
- Review date: 31 January 2026.
- Target audience: All staff who in the course of their work are required to know about the MCA deprivation of liberty (DoL) policy.
Page last reviewed: October 29, 2024
Next review due: October 29, 2025
Problem with this page?
Please tell us about any problems you have found with this web page.
Report a problem